Drug-induced liver injury (DILI) is responsible for drug attrition and 50% of cases of liver failures. Current models for drug toxicity include primary human hepatocytes (PHHs), hepatic cell lines, and animal models.
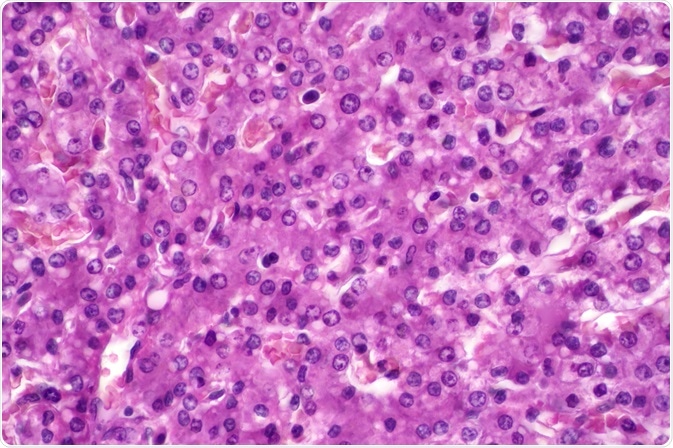
Image Credit: Choksawatdikorn/Shutterstock.com
Stem cell-derived hepatocytes present the opportunity to emulate the hepatocyte environment in vitro and provide a truer reflection of drug toxicity profiles. The advent of inducible pluripotent stem cells (hIPSCs) along with improved propagation techniques including 3-D culture provides for new opportunities in hepatotoxicity modeling.
History of hepatocytes
The architecture of the liver is very heterogeneous: composed of hepatocytes as well as supporting (non-Parenchymal) cells such as endothelial cells, Kuppfer cells (specialized macrophages), hepatic stellate cells, cholangiocytes and, Oval cells (progenitor cells). Hepatocytes are involved in lipid and carbohydrate metabolism, secretion of an array of factors as well as detoxification.
Hepatocytes also have a defined morphology and polarity: they exhibit a polygonal hepatic shape and possess bile canaliculi which facilitate extrusion. Modeling the complexity of the liver microenvironment is critical to recapitulate drug sensitivity in vivo.
hIPSCs provide an exciting alternative to the current models. The advent of new protocols facilitates the de-differentiation of somatic cells into stem cells; these can then be differentiated into Hepatocyte-Like cells (HLCs). These cells display a strong resemblance to PHHs, the current gold standard for drug toxicity modeling. They have been shown to be efficacious in terms of functions such as albumin secretion, Cytochrome P450 activity, and urea metabolism. Due to the inherent limitations of the current models, these hIPSC-HLCs will play a more critical role.
PHHs are limited in number, prone to de-differentiation, and display interindividual variability. Cell lines such as HepG2, HepaRG, and Fa2N-4 are often used as alternatives. These, however, are transformed cell lines and lack the genetic variation required for drug toxicity studies.
The gene expression of these cell lines is markedly different from that of PHHs. There is a failure amongst these models to detect the sub-clinical toxicity of known hepatotoxins such as paracetamol. Animal models such as rats and mice can fail to detect hepatotoxicity profiles due to species variations.
Improving HLCs
Techniques are being implemented to improve the viability, efficacy, and sensitivity of HLCs. Hepatocytes do not exist in a 2-D homogeneous environment in vivo. Co-culturing with other cells has been shown to enhance differentiation and proliferation including MEFS, adipose cells, 3T3 cells.
In order to emulate the 3-D environment, a variety of bespoke microfabrication techniques have been implemented. NanoPillar plates which possess nano-scaled micropatterned surfaces have been adopted to culture HLCs in the presence of Matrigel. This enhanced viability and allowed for the detection of hepatotoxins comparable to PHHs.
3-D bioprinting was implemented using Digital Light Processing to rapidly manufacture 3-D microstructures. HLCs cultured in this system displayed improved expression of critical CYP450 isoenzymes and greater response to rifampicin compared to 2-D culture.
One study utilized hIPSC-derived HLCs and hIPSC-derived endothelial cells using specific Interfacial Polyelectric Complex (IFC) fibers to bring these cells into the appropriate physiological spatial pattern. This involved the use of collagen I and galactose chitin conjugates for the HLCs and endothelial cells respectively in a Matrigel environment to mimic the in vivo microenvironment.
Concerns surrounding HLCs
A major concern with HLCs is the fetal hepatocyte phenotype it possesses; it expresses high levels of factors such as α-fetoprotein and CYP3A7. They also express diminished levels of critical CYP450 enzymes compared to PHHs. Modulation of factors enhances a mature phenotype.
Lipidomics revealed different lipid profiles as hepatocytes matured. Transcription factors such as Activating Transcription Factor 5 (ATF5), CCAATenhancer-binding protein-α (c/EBPα), and Prospero homeobox protein 1 (PROX1) are involved in the maturation of hepatocytes.
Lentiviral transfection of factors that promote a mature phenotype has improved this. Collagen I enhances a mature phenotype; PDMS micro-patterned with collagen improved maturity. A high-throughput screen of compounds showed laminin-411 as an important factor for improving HLC maturity.
MicroRNAs also modulate this. miR-122 is the most abundant miRNA in the liver and has been shown to be involved in differentiation from embryonic stem cells while inhibition of miR-199a-5p also enhanced differentiation.
Applications of hIPSC-derived hepatocytes
The most exciting aspects of hIPSC-derived hepatocytes are the opportunity to investigate idiopathic drug toxicity and model hepatic diseases. Monocyte-derived IPSCs have been shown to detect greater DILI sensitivity in patients, presenting diagnostic opportunities.
Pazopanib is a tyrosine kinase inhibitor used in chemotherapy which shows greater susceptibility to hepatotoxicity in some patients. iPSCs derived from different patients demonstrated variation in levels of the Cytochrome P450 isoform 1A2 and levels of glutathione depletion. One study concurrently assessed the drug sensitivity of PHHs and HLCs derived from those PHHs via pluripotent stem cell induction.
Interestingly, the inter-individual variation in CYP450 activity between PHHs corresponded to similar variations in the respective hIPSC-HLCs. This suggests that the stem cell-derived cells were able to reflect the individual drug responses. Analysis of the SNPs associated with the CYP2D6 isoform also confirmed that hepatotoxicity of the parent PHHs was recapitulated in the respective hiPSC-HLCs using tamoxifen.
hIPSCs derived from patients with specific rare diseases can recapitulate the disease phenotype. This is important for modeling the disease. In a model for Non-alcoholic fatty liver disease, supplementation of the culture with fatty acids facilitates the progression of the Non-alcoholic steatohepatitis phenotype. This is also critical for drug discovery.
Cardiac glycosides have been screened for familial hypercholesterolemia using hIPSC-HLCs. Five clinical drugs were identified for α-1-antitrypsin deficiency using patient-derived cells. NAD+ has been touted as a treatment for mtDNA deletion syndrome. The improved viability and scalability of hIPSC-HLCs allow high-throughput screening allowing for drug discovery and detection of drug sensitivity.
HLCs derived from hIPSCs present exciting new opportunities for disease modeling, drug toxicity, and clinical diagnostics of DILI. Challenges still must be overcome due to their immature phenotype, viability, and attenuated levels of critical enzymes involved in the three Phases of detoxification.
Optimization of culturing, microfluidics, and understanding of hIPSC-derived HLCs will only serve to better emulate the physiological environment of the hepatocyte and provide a better model for drug toxicity profiling.
Sources:
- Williams D. P. (2018). Application of hepatocyte-like cells to enhance hepatic safety risk assessment in drug discovery. Philosophical transactions of the Royal Society of London. Series B, Biological Sciences, 373(1750), 20170228. https://doi.org/10.1098/rstb.2017.0228
- Gurevich, I., Burton, S. A., Munn, C., Ohshima, M., Goedland, M. E., Czysz, K., & Rajesh, D. (2020). iPSC-derived hepatocytes generated from NASH donors provide a valuable platform for disease modeling and drug discovery. Biology Open, 9(12), bio055087. https://doi.org/10.1242/bio.055087
- Du, C., Narayanan, K., Leong, M. F., & Wan, A. C. (2014). Induced pluripotent stem cell-derived hepatocytes and endothelial cells in multi-component hydrogel fibers for liver tissue engineering. Biomaterials, 35(23), 6006–6014. https://doi.org/10.1016/j.biomaterials.2014.04.011
- Ma, X., Qu, X., Zhu, W., Li, Y. S., Yuan, S., Zhang, H., Liu, J., Wang, P., Lai, C. S., Zanella, F., Feng, G. S., Sheikh, F., Chien, S., & Chen, S. (2016). Deterministically patterned biomimetic human iPSC-derived hepatic model via rapid 3D bioprinting. Proceedings of the National Academy of Sciences of the United States of America, 113(8), 2206–2211. https://doi.org/10.1073/pnas.1524510113
- Schwartz, R. E., Fleming, H. E., Khetani, S. R., & Bhatia, S. N. (2014). Pluripotent stem cell-derived hepatocyte-like cells. Biotechnology advances, 32(2), 504–513. https://doi.org/10.1016/j.biotechadv.2014.01.003
Further Reading