Antibiotics have become a staple practice to cater for growing food demand, however, the rise of antibiotic-resistant bacteria, as well as the environmental consequences of antibiotics, has led to the gradual limitation of antibiotics in favor of alternatives.
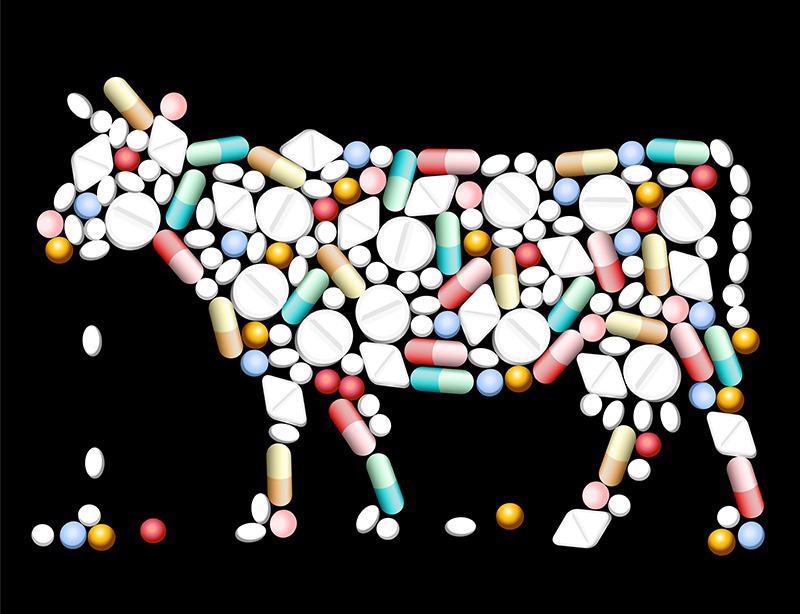
Image Credit: Peter Hermes Furian/Shutterstock.com
The use of antibiotics to remedy the rising demand for food
The global demand for food is expected to rise between 59% to 98% by 2050 due to the growth of human populations. In response to the rising pressures on global food security, agricultural practices have relied on ensuring productivity through various measures including antibiotics.
Antibiotics refer to a microbial‐derived compound that is active against bacteria. Both antibiotics and antimicrobials are often used interchangeably throughout literature although “antimicrobial” is mostly associated with resistance, whereas “antibiotic” is used when discussing a pharmacologically active agent.
Antibiotics, therefore, encompass several medications. Public and animal health institutions have created lists of “critically important antimicrobials” that rank these compounds according to their importance in human and veterinary medicine.
The WHO published its first list of critically important antimicrobials in 2005, and the most recent revision was released in 2019. Of the 260 drugs listed by the WHO list of antimicrobials, 39 are recommended or registered for use in cattle, swine, and poultry in the U.S. This includes drugs administered to individual animals and groups of animals to maintain their health as well as drugs used for growth promotion.
However, the use of antibiotics is not standardized across international guidelines. A 2019 review by Morgan Scott et al, discussed the use of multiple “critically important antimicrobial” lists and their contexts as created by various organizations. The review identifies discrepancies among these lists and describes issues surrounding risk management recommendations that have been made by regulatory organizations on the use of antibiotics in food animal production. The authors argue that standardized definitions are needed to identify shared contextual features, risk levels, and identify the best ways to maintain the health of food animals.
Nevertheless, antibiotics are widely used across agricultural practices from livestock maintenance to crop production.
The risks and rewards of antibiotic usage in agriculture
Within agricultural practices, antibiotics are used to minimize pain and treat disease, which is a core principle of animal husbandry and stands within the ‘five freedoms’ given to livestock. These freedoms include freedom from hunger and thirst; freedom from discomfort; freedom from pain, injury, and disease; freedom to express normal and natural behavior, and freedom from fear and distress.
Antibiotics also improve agricultural productivity as it allows the same amount of meat to be produced with fewer animals. In turn, greater efficiency results in less cropland area needed to grow animal feed decreased manure production, and further economic benefits for consumers (lower prices) and producers (greater profits).
However, despite these benefits, the extensive usage of antibiotics in agriculture has raised many concerns over recent years as it has resulted in the development of antibiotic-resistant bacteria as well as habitat degradation.
A common practice in the USA, approved by the United States Environmental Protection Agency, is to use streptomycin and oxytetracycline to limit diseases in plants and livestock. Streptomycin and oxytetracycline are used to control the spread of citrus greening disease, a bacterial disease caused by Candidatus Liberibacter asiaticus, as well as other infections such as Erwinia amylovora, which causes fire blight in apples, pears, and other related species. In addition, tetracycline antibiotics including oxytetracycline are used in animal husbandry and aquaculture to prevent harmful bacterial proliferation.
The widespread use of streptomycin and oxytetracycline has led to the rapid emergence of antibacterial resistant genes in various pathogens, which are able to thrive across livestock and crops and accelerate mutations favoring resistance genes due to overlapping usage of the antibiotic.
A 2018 study by Christy Manyi-Loh et al. discussed how antibiotic resistance is of great public health concern because the antibiotic-resistant bacteria associated with the animals may be pathogenic to humans, easily transmitted to humans via food chains, and widely disseminated in the environment via animal wastes.
In turn, the transmission of antibiotic-resistant pathogens may cause complicated, untreatable, and prolonged infections in humans, leading to higher healthcare costs and sometimes death. Moreover, the risk of transmission is also higher in less developed nations due to irrational use of antibiotics both in the clinical and agriculture settings, low socioeconomic status, poor sanitation, and hygienic status, as well as poor surveillance systems of resistant pathogens.
As a result, antibiotic usage has become increasingly scrutinized to prevent the development of harmful, untreatable, pathogens.

Image Credit: Lightspring/Shutterstock.com
The future use of antibiotics in agriculture
Although antibiotics contributed to the rise of food productivity in the 20th century, the use of such treatments is being increasingly limited in response to the rising concern of antibiotic-resistant pathogens.
However, the progress towards minimizing antibiotic usage is slow. Combined with the expected increase in pests and pathogens due to global climate change, researchers are attempting to develop alternative strategies to replace antibiotics or limit their impacts when used.
Indeed, researchers are developing new methods of administration. This is due to the fact that nearly 90% of the antibiotic administered orally may pass through the animal unchanged. The study by Kuldip Kumar et al., from 2005 presented how once excreted in urine and manure, these antibiotics can enter surface and/or groundwater through nonpoint source pollution from manure‐applied lands. The literature shows that most of the antibiotics are strongly adsorbed in soils and are not readily degraded, leading to habitat degradation as well as faster rates of antibiotic resistance in the environment.
This aligns with the use of vaccines to replace antibiotic usage, which allows direct administration to avoid environmental damage, and control infectious diseases with a reduced risk of protection development.
Specifically, various studies, including on by Hoelzer et al. from 2018, have demonstrated that vaccine usage in animal agriculture can lead to significant reductions in antibiotic consumption. To be effective, vaccines need to be widely used in food-producing animals, provide effective and long-lasting resistance, are easy to use, and cost-effective.
However, many current vaccines fall short in one or more of these respects. In response, scientific progress may overcome some of these limitations, by using mRNA vaccines for example, but development is funding-dependent and scarce in many regions.
Nonetheless, despite vaccines having the potential to improve animal health, safeguard agricultural productivity, and reduce antibiotic consumption, targeted research into the long-term uses of antibiotics and the development of alternatives is needed to avoid emerging issues including antibiotic-resistant bacteria.
Continue reading about the use of antibiotics in agriculture here.
Sources:
- Hoelzer, K., Bielke, L., Blake, et al. (2018). Vaccines as alternatives to antibiotics for food producing animals. Part 1: challenges and needs. Veterinary Research, 49(1). https://doi.org/10.1186/s13567-018-0560-8
- Kumar, K., C. Gupta, S., Chander, Y., & Singh, A. K. (2005). Antibiotic Use in Agriculture and Its Impact on the Terrestrial Environment. Advances in Agronomy, 1–54. https://doi.org/10.1016/s0065-2113(05)87001-4
- Manyi-Loh, C., Mamphweli, S., Meyer, E., & Okoh, A. (2018). Antibiotic Use in Agriculture and Its Consequential Resistance in Environmental Sources: Potential Public Health Implications. Molecules, 23(4), 795. https://doi.org/10.3390/molecules23040795
- Scott, H. M., Acuff, G., Bergeron, G., et al. (2019). Critically important antibiotics: criteria and approaches for measuring and reducing their use in food animal agriculture. Annals of the New York Academy of Sciences, 1441(1), 8–16. https://doi.org/10.1111/nyas.14058
Further Reading
Last Updated: Feb 25, 2022