For a long time, influenza scientists have largely focused their studies on the epithelial cells that line the lungs. This is because these cells are either destroyed or become infected while generating new copies of the virus.
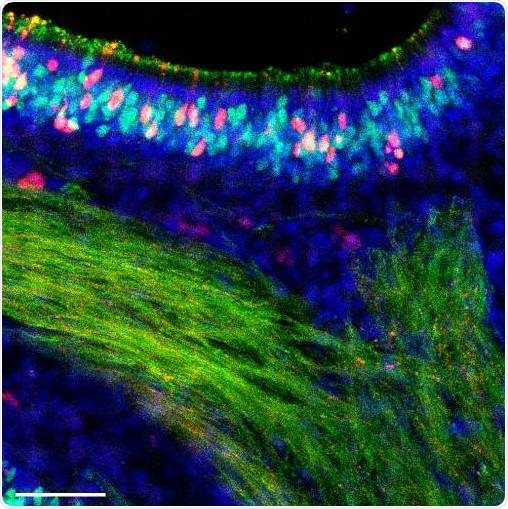
Fourteen days after infection with an influenza B virus, cells of a mouse nose are colored to show any remaining infection. Red cells were infected but have now cleared the virus. Image Credit: Sebastian Wellford, Moseman Laboratory, Duke University.
However, other cells that line the upper airways of the lungs are subjected to viruses in the same proportions and, in some way, may not possibly be destroyed by infections. It is not known whether this has to do with something the virus does or something that is done by those cells.
So you’re standing on the bus, somebody sneezes and you breathe something in. But where does that virus go? It's certainly not somehow sneaking all the way down to the bottom of your lungs before it encounters a cell. It’s hitting somewhere in your nose.”
Nicholas Heaton, Assistant Professor of Molecular Genetics and Microbiology, Duke University School of Medicine
In a study published in the Cell Reports journal on September 1st, 2020, an association between Heaton’s research team and Ashley Moseman’s laboratory in Duke Immunology reported on the notably strong immune reaction of olfactory sensory neurons—the smell receptors lining the nose, in which a virus might initially be encountered.
The team’s discoveries demonstrate an effective approach against infection and also highlight the diversity of immune reactions from one type of cell to another, added Heaton.
Olfactory neurons present a special danger of all the cells in the nose. This is because these neurons create a direct link from the airway to the nervous system. All viruses that gain control of that specific cell might gain entry to the central nervous system and the brain. Infections of the nervous system and the brain certainly occur in influenza; however, they are generally linked to “bird” flu strains.
Some years back, Heaton’s team published an article that showed that certain cells become infected by influenza but do not die.
Heaton added, “There’s this whole group of cells that get infected but do something different. So we felt like we should be studying those cells.”
Heaton also informed that his group wished to target the body’s initial contact with the virus in the upper respiratory tract and sinuses to observe if there were any variations in the immune reactions from one cell to another. The team noted that while the olfactory cells certainly become infected, they can combat the virus and prevent themselves from being killed by it.
Crucial to the discoveries was the capability to sort cells by type and subsequently carry out RNA sequencing that demonstrates the kind of genes that are active in a given type of cell. This enabled the team to visualize that the olfactory cells were stimulating a familiar set of genes to react to the invader, yet turning them up relatively higher (or relatively faster that they are not certain) than other types of cells do.
They upregulate genes that shut down viral replication, but the higher level to which they are induced was striking. It’s surprising, because most of these genes were discovered and best described in the respiratory cells.”
Rebekah Dumm, PhD Graduate, Duke School of Medicine
Dumm worked on this study as part of her thesis. This is the same group of antiviral genes utilized by the epithelial cells.
Olfactory neurons have the ability to fight this virus off a little better than other cells. We think that might be a brain protective mechanism.”
Nicholas Heaton, Assistant Professor, Department of Molecular Genetics and Microbiology, Duke University School of Medicine
Heaton added that it would be fair to question why all cells do not react to influenza in this manner; however, some tradeoff probably occurs that is still not evident. For instance, a powerful immune response that interrupted with air exchange would not appear to be a winning strategy.
Heaton further stated that his upcoming research work will continue to study the differences in immune response between cells.
“You’re a person who’s been exposed to all kinds of stuff, you have your own particular exposure history that gives you different antibodies, different cell memory phenotypes, probably also different epithelial phenotypes, and we’d like to know what that means in terms of how you respond to secondary infections or these types of things,” concluded Heaton.
Source:
Journal reference:
Dumm, R. E., et al. (2020) Heterogeneity of Antiviral Responses in the Upper Respiratory Tract Mediates Differential Non-lytic Clearance of Influenza Viruses. Cell Reports. doi.org/10.1016/j.celrep.2020.108103.