In this interview, AZoLifeSciences speaks to Professor Masaru Ishii about his latest research that investigated how bone marrow regenerates after chemotherapy.
What provoked your latest research into bone marrow?
The function of bone marrow-resident group 2 lymphoid cells (ILC2s) remained largely unknown. We newly found that bone marrow-resident ILC2s support the recovery of HSPCs from chemotherapy-induced stress by secreting GM-CSF.
ILC2s may function by 'sensing' the damaged BM spaces and subsequently support hematopoietic recovery under stress conditions.
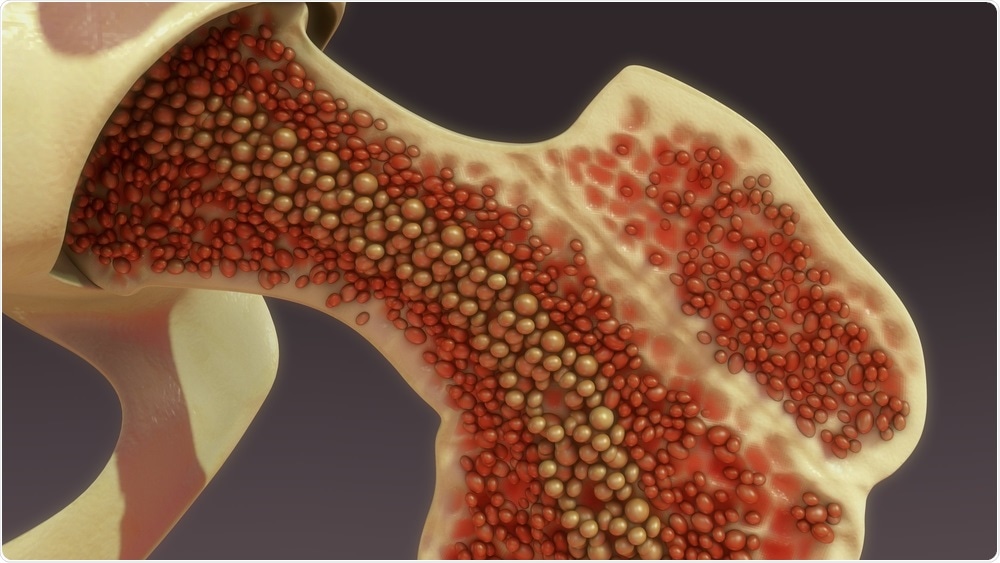
Bone Marrow. Image Credit: sciencepics/Shutterstock.com
Can you explain what chemotherapy is and how it damages hematopoietic stem and progenitor cells (HSPCs)?
Chemotherapy is widely used as an anti-cancer treatment. In the current article, we use 5-fluorouracil which has been used to treat various types of malignant diseases. While anti-cancer drugs mainly attack highly proliferative cancer cells, these drugs also target bone marrow cells undergoing cell division.
Since HSPCs are relatively quiescent cells compared to more differentiated cells, anti-cancer drugs usually damage mainly differentiated cells rather than hematopoietic stem and progenitor cells (HSPCs). We emphasize that surviving HSPCs become activated in cell-cycle status following chemotherapy to regenerate bone marrow cells.
What is the role of HSPCs in the body and why are they particularly sensitive to injury?
HSPCs in the bone marrow perpetually generate numerous hematopoietic cells, such as white blood cells, red blood cells, and platelets throughout our lifespan. As mentioned above, HSPCs are not particularly sensitive to chemotherapy.
Although they rarely undergo cell division, they become activated in cell-cycle status following chemotherapy to regenerate bone marrow cells.
Why has the regeneration process that HSPCs undergo remained a mystery until now?
Several studies have already been reported to elucidate the molecular mechanisms underlying bone marrow regeneration after chemotherapy-induced damage. For example, a study revealed that IL-6 produced by HSPCs is a particularly important regulator of myeloid differentiation and HSPC proliferation (Cell Stem Cell. 2014; 14(4): 445–459. doi:10.1016/j.stem.2014.01.007).
The critical trigger mechanisms occurring in the early stage have not been fully elucidated in part due to the phenotypic changes caused in HSPCs following acute BM stress, which makes it difficult to purify these cells from stressed BM.
Further, it would be challenging to clearly decipher whether the altered gene expression in HSPCs following BM stress is caused by cell-extrinsic or -intrinsic factors. To overcome this issue, we conducted unbiased comprehensive gene expression analysis, that allowed us to identify essential proliferative signals supplied from the damaged BM environment toward HSPCs.
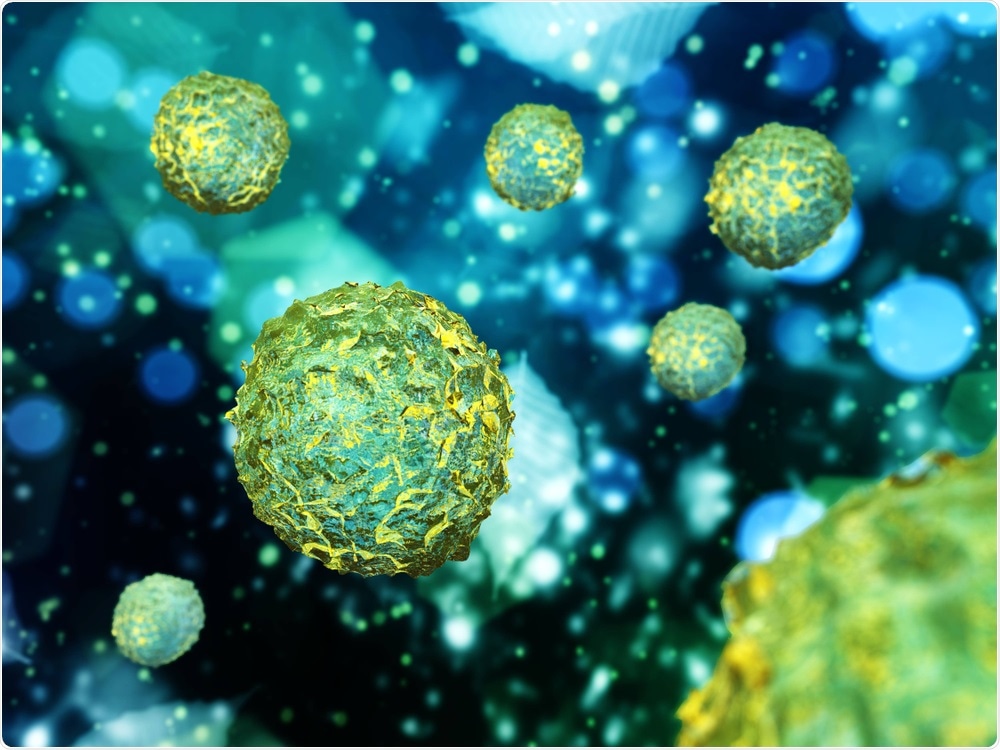
Hematopoietic Cells. Image Credit: ustas7777777/Shutterstock.com
Can you describe how you carried out your latest research into bone marrow and chemotherapy?
As mentioned above, we conducted unbiased comprehensive gene expression analysis (RNA-sequencing) of HSPCs that had homed into recipient bone marrow treated with or without 5-FU. The result of a bioinformatic analysis indicated that signals from GM-CSF were activated in HSPCs transplanted into 5-FU-treated mice.
We further revealed that GM-CSF protein in the BM was increased in response to 5-FU-treatment. These data suggested that a damaged microenvironment by 5-FU can promote the proliferation of transplanted HSPCs. We also performed a single cell-level gene expression analysis (single-cell RNA-seq analysis) to identify a specific cluster producing GM-CSF and found that ILC2s produced high amounts of GM-CSF.
What did you discover?
We discovered a function of bone marrow-resident ILC2s. We found that they support the recovery of HSPCs from chemotherapy-induced stress by secreting GM-CSF.
What other molecules are involved in the recovery of damaged bone marrow?
Previous reports have shown that IL-6 (doi:10.1016/j.stem.2014.01.007), FGF1 (doi:10.1038/nm.3706), and SCF, IL-1β, G-CSF, TGFβ, and CXCL4 (doi: 10.1038/nature21693) are involved in the recovery of damaged bone marrow.
Do you believe that your research will help us to improve current chemotherapy treatments?
While we have just discovered a mechanism of HSPC recovery in murine models, we hope that our findings are also applied in humans.
Our results implicate that adoptive transfer of cultured ILC2s might be a useful treatment to induce HSPC recovery after chemotherapy or bone marrow transplantation.

Chemotherapy. Image Credit: Numstocker/Shutterstock.com
What are the next steps in your research?
We are going to analyze human samples to develop a novel adjunct therapy aimed at early hematopoietic recovery.
Where can readers find more information?
About Professor Masaru Ishii
Masaru Ishii, M.D., Ph.D. (Professor of Immunology and Cell Biology, Graduate School of Medicine and Frontier Biosciences, Osaka University) was graduated from the Osaka University Medical School in 1998 and then worked as a physician specialized in rheumatology and internal medicine. He studied in the National Institutes of Health as a research fellow supported by the Human Frontier Science Program (2006-2008), as a laboratory chief in Osaka University Immunology Frontier Research Center (Associate Professor; 2008-2011, Professor; 2011-2013), and then appointed as a professor and chairman of the Department of Immunology and Cell Biology, Graduate School of Medicine, Osaka University, since 2013.
The bulk of his studies have so far elucidated the cellular dynamics in live bone tissues, with a special focus on bone-resorbing osteoclasts, by using intravital multiphoton-based bone imaging that he has originally developed. His study is not limited to the field of bone biology but is currently covering diverse research topics where cells are dynamically moving, such as immune cell migration in inflammatory sites and cancer invasion/metastases.
Dr. Ishii has authored over 100 publications in this field and has so far received several prestigious awards such as The Young Investigator Award, The Japanese Medical Association (2013), The JSPS Prize (2014), JSBMR Ogata Prize, The Japanese Society for Bone and Mineral Research (2018), Setsuro Ebashi Prize, The Japanese Pharmacological Society (2019), and Osaka Science Prize (2020).
He serves as the Vice President of the Japanese Society for Bone and Mineral Research, as an Executive Board Member of the International Federation of Musculoskeletal Research Societies, and also serves as the Trustees for the Japanese College of Rheumatology and the Japanese Society of Inflammation and Regeneration.