Scientists at the Francis Crick Institute have revealed how a mechanism involved in the regeneration of tissue—damaged by radiation—can help the spread of cancer.
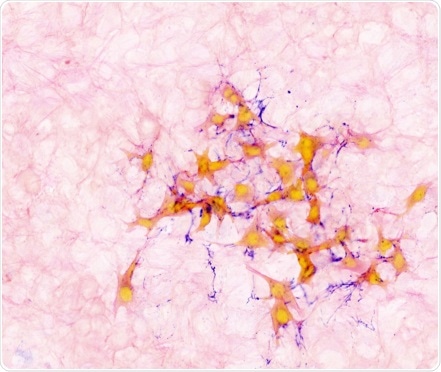
Image showing mouse breast cancer cells (orange) within lung tissue (light pink) connected with protein fibers (purple). Image Credit: The Francis Crick Institute.
The spreading of cancer throughout the body is a complicated process and knowing more about the process is important to the development of new therapies.
The research team investigated the association between healthy tissue repair and the growth of cancer in its study that was published on February 24th, 2022, in the Nature Cancer journal.
Researchers exposed healthy mouse lungs—a location where many cancers spread more commonly—to a high dosage of radiation to affect the tissue. Then, they tested the possibility of breast cancer cells growing in the damaged area relative to the uninjured lungs. More cancer cells pass on to the lungs and start forming secondary tumors in mice, which had been injured by radiation in comparison to the mice that had not been injured.
More experiments showed that this is due to the signaling of neutrophils—a sort of immune cell—which aids in repairing tissue damage. Secondary tumors were greatly decreased when the scientists obstructed signaling from the neutrophils in the affected lungs.
This is a situation where tissue damage sets the stage for the spread of cancer and, in trying to repair the damaged tissue, the immune system inadvertently aids the cancer. This role of neutrophils in supporting cancer spread is something which needs further research and could potentially help to identify new ways to treat the disease.”
Emma Nolan, Study First Author and Post Doctoral Fellow, Tumour-Host Interaction Laboratory, The Francis Crick Institute
“The relationship between cancer cells, the immune system, and the organ where cancer takes hold is highly complex. And it’s by untangling aspects of this web that we can better understand why cancer is able to spread, what predisposes organ to the arrival of cancer cells, and ultimately how we can try to stop this,” remarks Ilaria Malanchi, study author and group leader of the Tumour-Host Interaction Laboratory.
It is essential to note that, in this study, the mice were exposed to radiation of a higher dose than that is used for radiotherapy in the hospital and targeted a considerably greater proportion of the tissue. Owing to advancing technology, radiation exposure is now limited to cancerous tissue and radiotherapy serves as a strong tool to control cancer disease.
Unrevealing the new responses of neutrophils to radiation we described here, could further enhance the efficacy of this highly-regarded treatment for cancer.”
Ilaria Malanchi, Study Author and Group Leader, Tumour-Host Interaction Laboratory, The Francis Crick Institute
Source:
Journal reference:
Nolan, E., et al. (2022) Radiation exposure elicits a neutrophil-driven response in healthy lung tissue that enhances metastatic colonization. Nature Cancer. doi.org/10.1038/s43018-022-00336-7.