Scientists are reprogramming the immune system through cutting-edge approaches like CAR-T cells, engineered dendritic vaccines, AI-driven antibody design, and senolytic therapies, highlighting both the revolutionary potential and the ethical, clinical, and biological risks of reshaping human immunity.
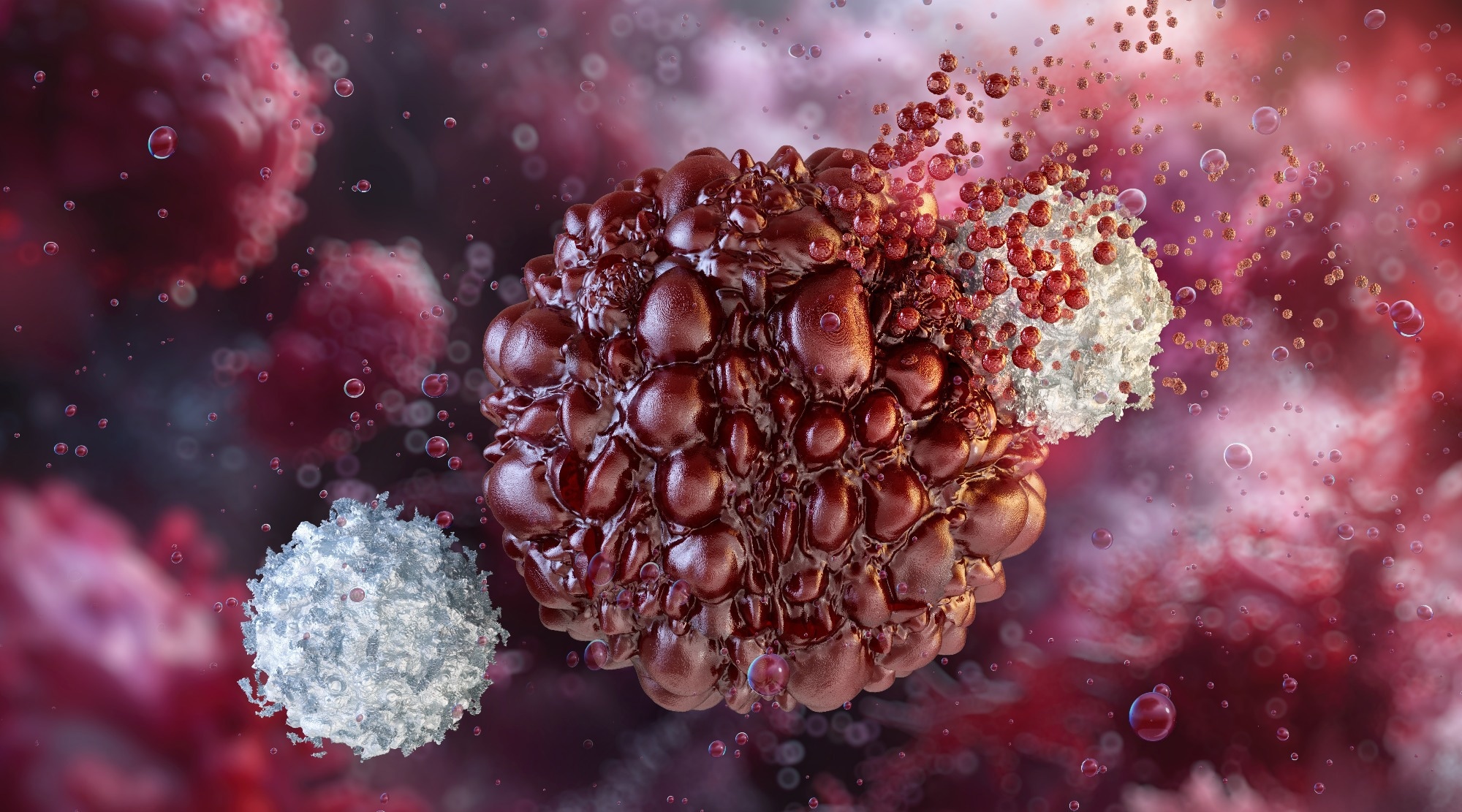 Image credit: Corona Borealis Studio/Shutterstock.com
Image credit: Corona Borealis Studio/Shutterstock.com
Introduction
The immune system primarily functions to eliminate invading and foreign organisms such as pathogens and tumour cells. However, the immune system is also responsible for more complex functions like tissue repair after injury. All these integrated processes are involved in maintaining homeostasis1.
The ability to manipulate the immune system has been trialled since the 18th century, where vaccines that modulated cellular responses to protection against infections were first developed. However, the shift has recently been to ‘re-educate’ the immune system to combat cancer and disease1.
CAR-T Cell Therapy
Immune reprogramming is essential in cancer treatment development. Conventional treatments have moderate success with high rates of recurrence and poor prognosis, so immunotherapy has evolved as a potential solution to these challenges2.
Chimeric antigen receptor-T (CAR-T) cell therapy is an approach that uses CARs, which are ‘synthetic transmitters’ with antigen recognition domains to activate T lymphocytes (a subset of immune cells stimulated as part of the natural adaptive immune response against tumour cells)3,4.
The CAR-T cells bind to the target protein on the tumour cell surface to trigger a signalling cascade, like the natural T-cell activation. Then, CAR-T cells can release cytotoxins or interferon γ and tumour necrosis factor α, leading to lysis and death of the tumour cell or stimulation of the inflammatory response, respectively. Activated CAR-T cells also activate other immune cells to form an ‘alliance’ that targets tumour cells.
This therapy has reported many successful results, particularly in targeting CD19+ leukaemia cells and relapsed B-cell non-Hodgkin’s lymphoma. Depending on disease subtype and treatment protocol, approximately 50-80% of patients achieve remission.
CAR-T cell therapy has shown notable efficacy but has many associated side effects. One of the most common is cytokine release syndrome (CRS), which occurs in over 50% of patients (with 8-18% experiencing severe forms). CRS is the overactivation of the immune system, leading to systemic inflammation, manifesting as fever, nausea, chills, difficulty breathing, and, in more severe cases, anaemia and thrombocytopenia.
Other side effects include downregulating antigen expression caused by tumours, leading to resistance, or ‘on-target off-tumour effects. Here, the CAR-T cells target non-tumor cells that express the target antigen. Although one of the most successful therapies to be implemented and result in long-term remission, its efficacy is limited due to the heterogeneity of tumours, making it harder for the CAR-T cells to recognise antigens.
Additionally, a lot of patients experience relapse or drug resistance4. Recent efforts focus on next-generation CAR designs and combination therapies to improve the safety and durability of response.
A Look at How CAR-T Cell Therapy Works
Video credit: AssociatedPress/Youtube.com
Engineered Dendritic Cells as Cancer Vaccines
Another promising immune reprogramming approach involves engineered dendritic cells (DCs), which act as powerful antigen-presenting cells capable of priming T-cell responses. In cancer immunotherapy, DCs can be loaded ex vivo with tumour antigens or genetically modified to express co-stimulatory molecules that enhance antigen presentation. These reprogrammed cells are then reintroduced into patients to stimulate targeted antitumour immunity.
Early clinical trials have demonstrated that engineered DC vaccines can elicit durable immune responses in melanoma, glioblastoma, and prostate cancer. However, their overall efficacy has been modest, often limited by tumour-induced immunosuppression and variability in DC maturation protocols. Ongoing studies explore combination strategies that pair DC vaccines with checkpoint inhibitors or adjuvants to overcome these barriers5.
Aging and Inflammaging
A decline in immune system function, called senescence, characterizes aging, where normal cells block proliferation, resulting in inflammaging6. This is chronic inflammation due to a weakened immune system, which impairs its ability to combat inflammatory responses and detect pathogens. Chronic inflammaging is caused by multiple factors, such as damage-associated molecular patterns (DAMPs) and gut microbiota dysregulation. As a result, tissue damage and age-related diseases such as cardiovascular disorders and neurodegeneration are exacerbated7.
Immune reprogramming therapies target the main mechanisms that cause inflammaging and restore balance to the aging process. An example is thymus rejuvenation, which aims to restore thymus function, which is severely affected during aging. T lymphocytes and thymic epithelial cells (TECs), responsible for T-cell differentiation, are reduced. Overexpression of a transcription factor, FOXN1, which maintains TECs and declines with age, has been shown to restore this function and promote T cell production7.
Another promising therapy to combat senescent cells (SnCs) and the onset of inflammaging is the development of senolytics. Senolytics target senescent Cell Anti-Apoptotic Pathways (SCAPs). Well-characterised senolytic drugs include a combination of Dasatinib (D), a tyrosine kinase receptor inhibitor, and Quercitin (Q), a compound that targets BCL-2, a critical apoptotic protein6,8. This combination is the most effective at targeting different types of SnCs, part of ‘pro-survival’ pathways, particularly in chronic kidney disease, idiopathic pulmonary fibrosis (IPF), and Alzheimer’s disease6.
Senolytic drugs can effectively combat age-related senescence and inflammaging; however, only a few trials have evaluated their efficacy in humans. This includes using a combination of D and Q, where participants, at risk of Alzheimer’s disease, showed improved cognition and mobility9.
Autoimmunity and Immune Overactivation
While immune reprogramming offers therapeutic promise, it also risks tipping the immune balance toward autoimmunity. Modifying immune checkpoints or enhancing immune cell activation can sometimes lead to unintended attacks on healthy tissues. For instance, CAR-T cell therapy has been associated with off-target toxicities and cytokine-mediated tissue damage that resemble autoimmune reactions. Similarly, checkpoint blockade therapies can trigger autoimmune-like side effects such as colitis or thyroiditis. As new strategies are developed to rejuvenate or redirect immune function, careful monitoring and modulation of immune tolerance mechanisms will be critical to minimize these risks10.
AI-designed antibodies & vaccines
A new concept in the field of immune re-programming is artificial intelligence (AI). Vaccine development has utilised AI to tackle traditional methods, which make the process expensive and time-consuming. AI uses machine learning and deep learning to analyse genomic, protein, and immune system interactions to predict epitopes, assess immunogenicity, and select target antigens. For example, during the COVID-19 pandemic, AI algorithms identified novel antigens for the various vaccines, allowing a rapid response to the pandemic11–13.
 Image credit: Ground Picture/Shutterstock.com
Image credit: Ground Picture/Shutterstock.com
Monoclonal antibodies have been crucial in advancing molecular and cellular biology as they can target specific and unique antigens, leading to over 170 approved antibody therapeutics worldwide. Using computational and structural biology, AI can predict protein structure and sequence14.
The use of AI is proving to be extremely useful, but several aspects raise ethical and legal concerns. For instance, AI results in a ‘black box’ effect, a lack of transparency and clarity regarding the ‘decision-making’ processes and algorithms used to design antibodies/vaccines. This is essential for patent registration and application, particularly for vaccines.
Further problems arise related to intellectual property (IP) rights, which are usually assigned to humans, but it remains uncertain whether AI inventions can be patented legally15. Moreover, translating AI predictions into clinically validated immune therapies requires rigorous experimental validation and regulatory oversight. Overall, AI-designed biological and pharmaceutical products may be helpful to immunology, but remain a grey area in several aspects.
Conclusion
Immune reprogramming encompasses multiple strategies that may enable humans to combat challenging diseases as serious as cancer or even natural processes such as aging. However, although some of the treatments and therapies described here are well established, many require thought and further development to ensure that reprogramming our immune systems is an ethical and safe process.
Balancing innovation with safety and immune tolerance will ultimately determine how effectively these approaches translate into clinical reality.
References
- Placek K, Schultze JL, Aschenbrenner AC. Epigenetic reprogramming of immune cells in injury, repair, and resolution. Journal of Clinical Investigation 2019;129(8):2994–3005.
- Mavi AK, Gaur S, Gaur G, Babita, Jindal P, Kumar N, et al. CAR T-cell therapy: Reprogramming patient’s immune cell to treat cancer. Cell Signal 2023; 105:110638.
- Dong Y, Wan Z, Gao X, Yang G, Liu L. Reprogramming Immune Cells for Enhanced Cancer Immunotherapy: Targets and Strategies. Front Immunol 2021;12.
- Sun D, Shi X, Li S, Wang X, Yang X, Wan M. CAR‑T cell therapy: A breakthrough in traditional cancer treatment strategies (Review). Mol Med Rep 2024;29(3):47.
- Pérez CR, Teijeira Á, et al. “Engineering dendritic cell vaccines to improve cancer immunotherapy.” Nat. Commun. 2019;10:5408
- Lelarge V, Capelle R, Oger F, Mathieu T, Le Calvé B. Senolytics: from pharmacological inhibitors to immunotherapies, a promising future for patients’ treatment. npj Aging 2024;10(1):12.
- Nguyen TQT, Cho KA. Targeting immunosenescence and inflammaging: advancing longevity research. Exp Mol Med 2025;57(9):1881–92.
- Vogler M, Braun Y, Smith VM, Westhoff MA, Pereira RS, Pieper NM, et al. The BCL2 family: from apoptosis mechanisms to new advances in targeted therapy. Signal Transduct Target Ther 2025;10(1):91.
- Millar CL, Iloputaife I, Baldyga K, Norling AM, Boulougoura A, Vichos T, et al. A pilot study of senolytics to improve cognition and mobility in older adults at risk for Alzheimer’s disease. EBioMedicine 2025; 113:105612.
- Song Y, Ding J, et al. “Evolving understanding of autoimmune mechanisms and immunotherapies.” Sig. Transduct. Target Ther. 2024;9:45.
- Abdelmageed MI, Abdelmoneim AH, Mustafa MI, Elfadol NM, Murshed NS, Shantier SW, et al. Design of a Multiepitope‐Based Peptide Vaccine against the E Protein of Human COVID‐19: An Immunoinformatics Approach. Biomed Res Int 2020;2020(1).
- Sharma A, Virmani T, Pathak V, Sharma A, Pathak K, Kumar G, et al. Artificial Intelligence‐Based Data‐Driven Strategy to Accelerate Research, Development, and Clinical Trials of COVID Vaccine. Biomed Res Int 2022;2022(1).
- Olawade DB, Teke J, Fapohunda O, Weerasinghe K, Usman SO, Ige AO, et al. Leveraging artificial intelligence in vaccine development: A narrative review. J Microbiol Methods 2024; 224:106998.
- Vecchietti LF, Wijaya BN, Armanuly A, Hangeldiyev B, Jung H, Lee S, et al. Artificial intelligence-driven computational methods for antibody design and optimization. MAbs 2025;17(1).
- Zumárraga J, McConnell MJ, López D, Martín-Galiano AJ. Legal questions of AI-generated immunological products for infectious diseases. Hum Vaccin Immunother 2025;21(1).
Last Updated: Nov 13, 2025