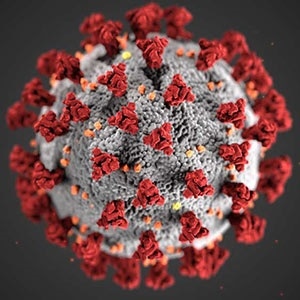
Sars-CoV-2 virus, which causes COVID- Image Credit: CDC / Alissa_Ecker_MS; Dan_Higgins, MAMS.
The researchers found that within the nose, ciliated and goblet cells contain the entry proteins in increased concentrations, which are leveraged by the COVID-19 virus to enter into an individual’s cells.
The first publication, reported in Nature Medicine journal on April 23rd, 2020, with the Lung Biological Network is part of an ongoing global effort to utilize the Human Cell Atlas data to learn more about the disease and infection.
The publication further demonstrated that viral-entry proteins are also present in the cells located in the eye and some other organs.
In addition, the research predicts the way a key entry protein is controlled with other immune system genes and shows the possible targets for developing novel treatments to minimize its transmission.
COVID-19 is a novel coronavirus disease that mainly affects the airways and lungs. Patients can develop flu-like symptoms such as coughing, fever, and sore throat. Some individuals may not experience symptoms but will still have the transmissible virus.
In the worst scenario, the virus leads to pneumonia that can eventually cause death. It is believed that the virus spreads via respiratory droplets that are created when an infected person sneezes or coughs and seems to be easily transmitted within the affected regions. To date, the virus has been spread to over 184 nations and caused the death of more than 178,000 persons.
Globally, researchers are making efforts to understand the exact spreading mechanism of the virus, so that its transmission can be prevented and to a potential vaccine can be developed.
The virus that causes the COVID-19 disease, also called SARS-CoV-2, employs a mechanism to infect the human cells similar to coronavirus that caused the SARS epidemic in 2003, but the exact types of cells involved in the nose had not been identified before.
The researchers examined multiple Human Cell Atlas§ (HCA) associated datasets of single-cell RNA sequencing to find out the type of cells that may be involved in the transmission of the COVID-19 virus.
These datasets were taken from over 20 different tissues of non-infected people. These comprised cells from the eye, nasal cavity, lung, liver, kidney, and gut.
The team searched for individual cells expressing the two major entry proteins, which were utilized by the COVID-19 virus to infect the human cells.
We found that the receptor protein—ACE2—and the TMPRSS2 protease that can activate SARS-CoV-2 entry are expressed in cells in different organs, including the cells on the inner lining of the nose.”
Dr Waradon Sungnak, Study First Author, Wellcome Sanger Institute
Sungnak continued, “We then revealed that mucus-producing goblet cells and ciliated cells in the nose had the highest levels of both these COVID-19 virus proteins, of all cells in the airways. This makes these cells the most likely initial infection route for the virus.”
This is the first time these particular cells in the nose have been associated with COVID-19. While there are many factors that contribute to virus transmissibility, our findings are consistent with the rapid infection rates of the virus seen so far. The location of these cells on the surface of the inside of the nose make them highly accessible to the virus, and also may assist with transmission to other people.”
Dr Martijn Nawijn, University Medical Center Groningen
Dr. Nawijn made the above statement on behalf of the HCA Lung Biological Network.
The two major entry proteins, named TMPRSS2 and ACE2, were also detected in the cells present in the eye’s cornea and also in the intestine lining. This implies an alternative route of infection through the tear ducts and eye and also demonstrated a potential for fecal-oral transmission.
When cells are fighting an infection and become damaged in the process, activation of various immune genes occurs. This research proved that the production of the ACE2 receptor in the nose cells is likely to be turned on simultaneously as the other immune genes.
The study was performed as part of the global Human Cell Atlas consortium, the aim of which is to design reference maps for all human cells to interpret both the health and disease.
Over 1,600 persons across 70 nations were involved in the HCA community, and the information is openly accessible to researchers around the world.
Dr. Sarah Teichmann stated, “As we’re building the Human Cell Atlas it is already being used to understand COVID-19 and identify which of our cells are critical for initial infection and transmission. This information can be used to better understand how coronavirus spreads. Knowing which exact cell types are important for virus transmission also provides a basis for developing potential treatments to reduce the spread of the virus.”
Dr. Teichmann is a Senior Author from the Wellcome Sanger Institute and co-chair of the HCA Organizing Committee.
The global HCA Lung Biological Network continues its analysis of the data to offer an additional understanding of the cells and targets that could be involved in the COVID-19 pandemic and to relate them to the characteristics of the patient.
By pinpointing the exact characteristics of every single cell type, the Human Cell Atlas is helping scientists to diagnose, monitor and treat diseases including COVID-19 in a completely new way. Researchers around the world are working at an unprecedented pace to deepen our understanding of COVID-19, and this new research is testament to this. Collaborating across borders and openly sharing research is crucial to developing effective diagnostics, treatments and vaccines quickly, ensuring no country is left behind.”
Sir Jeremy Farrar, Professor and Director, Wellcome Sanger Institute
Source:
Journal reference:
Sungnak, W., et al. (2020) SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nature Communications. doi.org/10.1038/s41591-020-0868-6.