UC San Francisco researchers have defined 12 classes of “immune archetypes” to identify cancer tumors based on data from over 300 patient tumors. Their findings, published in Cell this week, show that tumors from diverse areas of the body are immunologically identical. These categories provide distinct methods for improving each patient’s cancer immunotherapy options.
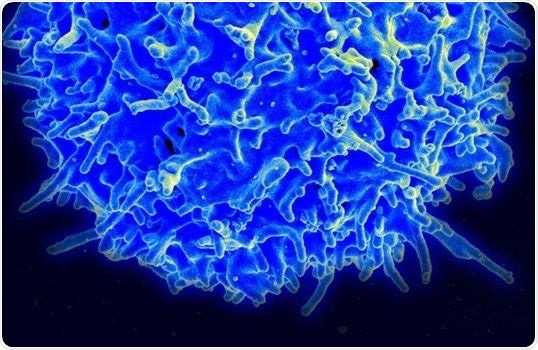
Microscopic image of a human T cell. T cells are the focus of current immunotherapies, however, researchers found that tumors contain a wide range of other immune cells, such as macrophages, NK and B cells. Image Credit: National Institutes of Health.
The UCSF team, headed by first co-authors Alexis Combes, Ph.D., and Bushra Samad, MS, as well as senior author Max Krummel, Ph.D., acquired tumor specimens from 78 UCSF doctors and reviewed 364 tumor samples from patients, dividing them into groups based on their immune microenvironment.
Their findings provide a novel approach to cancer immunotherapy that takes into account the immunological environment surrounding the tumor and leads to customized immunotherapies.
This is a new framework for how to look at cancer patients. This work will help clinicians find the right biology to target and avoid targeting cells that aren’t present in the tumor.”
Alexis Combes, Director, D2B CoLab and Incoming Assistant Professor, Department of Pathology, University of California–San Francisco
Immunotherapy for cancer treatment utilizes the body’s immune system to fight the disease. It is promising for it was first introduced as a biological therapy for the treatment of different cancers. Immunotherapy has shown to be effective in certain people, but it is not effective in all patients.
“We were driven by this question of why immunotherapies work for some people and not others. It’s more complex than responders and non-responders. Our goal was to discern how many responses there are to these targeted therapies.” added Krummel, Robert E. Smith Endowed Chair in Experimental Pathology and director of the Krummel Lab at UCSF.
Tumors have microenvironments
Tumors are not simply out-of-control cells. They are also packed with immune cells that are meant to destroy cancer cells. On the other hand, malignant cells, in cancer, are capable of overcoming the body’s immunological response and continue to develop.
A team of researchers discovered a variety of malignancies are seen in prescribed forms, each of which indicates a distinct subversion of the body’s immune systems. The researchers classified various microenvironments in the tumors, examining which immune cells were present and which genes were expressed.
Combes stated, “We could see that the tumors and their environments inform each other.”
The researchers were able to classify the tumors into 12 categories, which they refer to as archetypes. What amazed the researchers was that the tumors contained a wide spectrum of immune cells, such as B cells, macrophages, and NK which are beyond the T cells that are the focus of present immunotherapies.
According to their findings, a tumor’s immunological archetype is not always related to the kind of cancer. Some archetypes are based mostly on a few cancer types. Others make use of a diversity of ways. This indicates that certain melanomas are similar to lung tumors but differ biologically from that of others.
Unbiased interrogation of multiple data sources including genetic sequencing, cell surface markers, imaging, and patient clinical data, set the groundwork atop which we were able to identify and describe these immune archetypes.”
Bushra Samad, Assistant Professor, Department of Pathology, University of California–San Francisco
Identifying patients for clinical trials
The classification system not only determines which tumors are likely to be sensitive to existing immunotherapies, but it also aids in determining which patients would respond best to which clinical trial.
“This architecture allows us to get rid of a lot of noise. It’s possible that we were destroying cells that weren't even in the tumor,” Krummel added.
Krummel’s study team was able to collect a huge group of UCSF scientists and doctors—a total of 78—who contributed knowledge from a variety of disciplines. The authors joined together intending to boost the levels of promising therapies. The CoLabs at UCSF fosters this dual vision and a large body of knowledge.
This is just the beginning of this project. We believe this is the next step in personalized medicine for cancer therapy. When the immunotherapy you design can thus be placed against the correct biology. That biology may not always go by a name we have heretofore known. Archetypes, we think, are those names.”
Matthew F. Krummel, Assistant Professor, Department of Pathology, University of California–San Francisco
1264680_PanCancerAnimation_010522.mp4
Video Credit: Krummel Lab.
Source:
Journal reference:
Combes, A. J., et al. (2021) Discovering dominant tumor immune archetypes in a pan-cancer census. Cell. doi.org/10.1016/j.cell.2021.12.004.