 By Pooja Toshniwal PahariaReviewed by Lauren HardakerOct 2 2025
By Pooja Toshniwal PahariaReviewed by Lauren HardakerOct 2 2025In a recent study published in Scientific Reports, researchers combined four-dimensional (4D) flow magnetic resonance imaging (MRI) with three-dimensional printing to map blood flow in a pulsating total artificial heart (TAH) in an MRI-compatible mock circulatory loop under representative conditions.
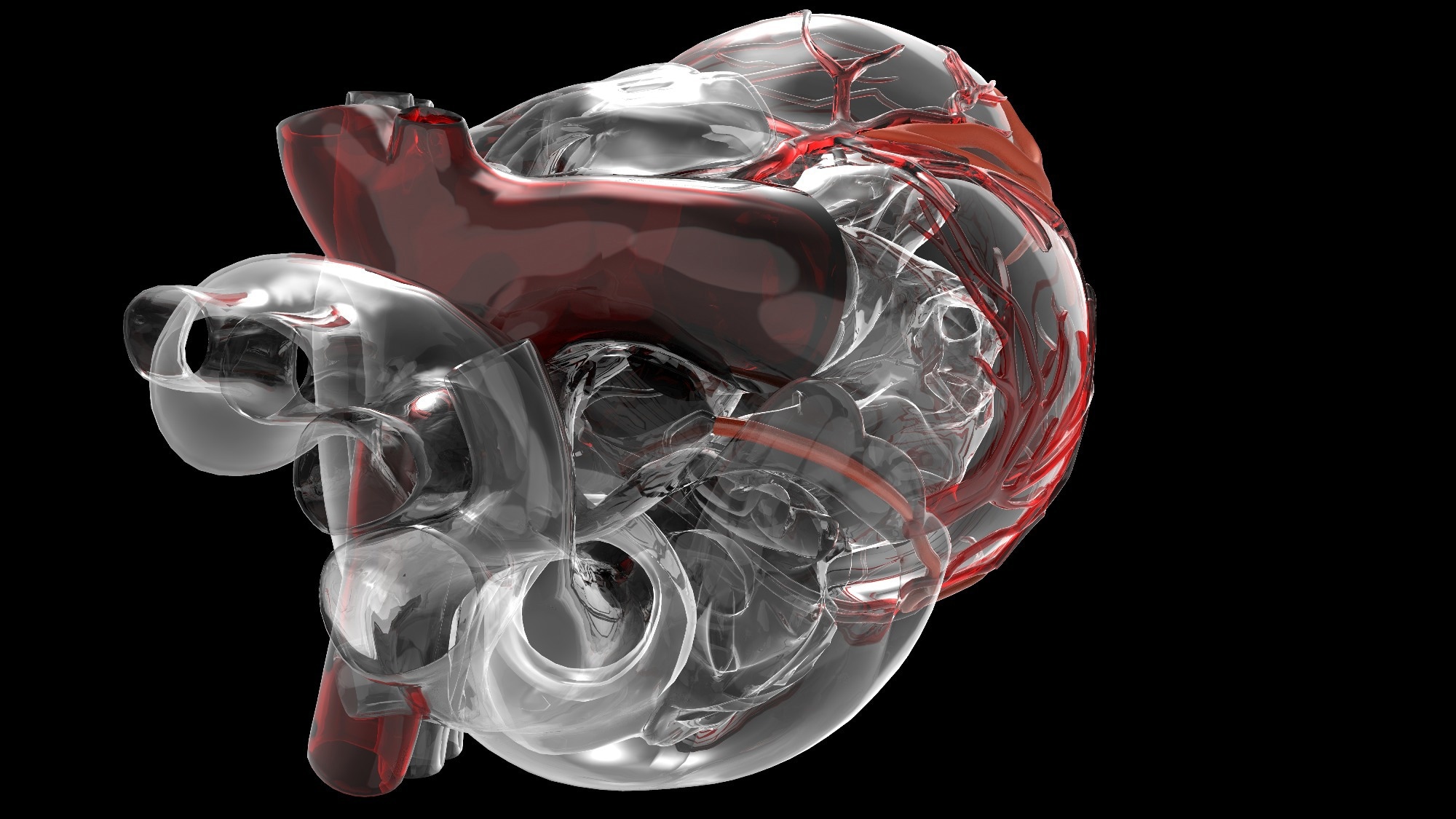 Image credit: Dariush M/Shutterstock.com
Image credit: Dariush M/Shutterstock.com
The TAH demonstrated stasis, turbulence, and energy loss with high-quality, time-resolved measurements (with known limitations near valves and for viscous-dissipation maps), providing critical quantitative insights to guide iterative design improvements. The method highlights a powerful tool for developing safer, more effective TAHs for patients with end-stage heart failure, a necessity due to donor heart shortages.
Heart transplantation remains the gold standard for end-stage heart failure, yet donor shortages leave many patients without access to needed treatment. TAHs offer an alternative, but complications such as infection, hemolysis, and stroke, primarily driven by adverse flow changes, limit current devices. To advance TAHs from bridge-to-transplant toward destination therapy, improved evaluation of flow patterns is essential.
Computational and conventional experimental methods face challenges in capturing complex pulsatile flow. Four-dimensional flow MRI provides a powerful, non-invasive tool to quantify stasis, turbulence, and energy loss, offering critical insights to improve TAH design and safety.
About The Study
In the present study, researchers examined the practicability of performing 4D flow MRI to evaluate blood flow characteristics in a pulsatile-type TAH prototype under clinically representative conditions. For MRI compatibility, they adapted a left-sided pulsatile TAH prototype (RealHeart v11c, Scandinavia).
They replaced ferromagnetic parts with 3D-printed components and relocated the motor 2.5 m outside the MRI bore via an extended drive shaft. Non-ferromagnetic bi-leaflet valves were used to maintain normal function, with minimal local image loss accepted.
The researchers connected the modified TAH to a closed, MRI-appropriate artificial circulatory loop, simulating left-sided heart pressures. The system comprised silicone tubing with compliance and pressure chambers to simulate atrial filling. They regulated pressures hydrostatically and through adjustable resistance, with catheters and sensors monitoring inflow and outflow for validation. A mixture of water and glycerol (density 1,089 kg/m³; viscosity 3.7 × 10⁻³ kg·m⁻¹·s⁻¹) replicated blood, while a gadobutrol contrast agent improved imaging.
The team monitored heart function using dedicated software, adjusting for rate and filling parameters. They performed experiments at heart rates of 80, 105, and 120 beats per minute (bpm) with stroke volume maintained at 55 mL. To simulate physiological conditions, they maintained aortic and atrial pressures of 110 mmHg and 10 mmHg, respectively.
The researchers obtained flow measurements using a 3.0 T MRI system with 16-channel head coils and electrocardiogram (ECG) gating. Two velocity encoding settings captured the mean flow and turbulence, yielding images with an isotropic spatial resolution of 2.0 mm and a 23–25 ms temporal resolution.
The researchers quantified flow using several key metrics: Reynolds number, blood stasis (velocity below 0.1 m/s), viscous energy loss, turbulent kinetic energy (TKE), and shear stress, all factors clinically linked with hemolysis and thrombosis. In addition, particle pathlines and maximum intensity projections mapped flow structures like vortices and recirculation zones, helping to identify regions that may pose a risk for blood damage.
Results
The MRI-compatible pulsatile TAH produced high-quality, time-resolved velocity and turbulence measurements in nine minutes of scanning. Flow pathline visualizations revealed physiologically relevant structures across the cardiac cycle, including recirculation during filling, Dean vortices in the atrioventricular (AV) cylinder, a vortex ring in the ventricle, and recirculation at the 90° outflow bend. The features closely resemble flow patterns seen in native hearts and point to potential regions where blood damage may occur.
Volumetric flow analysis revealed strong agreement between inlet and outlet volumes, with stroke volume differences of 0.4 to 4.6 mL. At heart rates ranging from 80 to 120 bpm, mean cardiac output rose from 4.1 to 6.2 liters per minute. Stasis decreased as heart rate increased, and atrial stasis values (7 to 17%) were similar to those reported in healthy controls. Importantly, no regions demonstrated complete stasis.
Viscous energy loss rose with an increasing heart rate but stayed within ranges typical of healthy ventricles and considerably lower than in disease. Scalar shear stress followed a similar trend, increasing modestly but remaining low overall, peaking at 1.4 Pa, well below thresholds associated with hemolysis.
Elevated TKE values were observed in the atrium, ventricle, and outflow tract. The highest peak, 240 J/m³ at 120 bpm, occurred at the outflow bend, comparable to values observed in older healthy subjects and lower than levels reported in patients with severe valvular disease. Integrated TKE values in the atrium and ventricle were slightly higher than in healthy controls, but remained significantly lower than those among individuals with pulmonary regurgitation or hypertrophic cardiomyopathy.
Based on the findings, 4D flow MRI enables the precise assessment of pulsatile TAH hemodynamics in a left-sided prototype within a mock loop, with stasis, energy loss, and shear stress comparable to healthy hearts and turbulence magnitude comparable to older healthy subjects and lower than disease cohorts. The study approach supports rapid design iteration, computational fluid dynamics (CFD) validation, and future blood-damage prediction with advanced turbulence mapping.
Journal Reference
Bakker, T., Najar, A., Finocchiaro, T., et al. (2025). 4D flow MRI enhances prototype testing of a total artificial heart, Sci Rep., 15, 32533. DOI: 10.1038/s41598-025-18422-y. https://www.nature.com/articles/s41598-025-18422-y