Autoantibodies are a subset of antibodies that bind to cell-surface proteins in the host’s cells, as opposed to the antigens of foreign cells or viral proteins. This is the cause of many different autoimmune diseases such as type I diabetes and rheumatoid arthritis.

Image Credit: Puwadol Jaturawutthichai/Shutterstock.com
They are created by the body as a result of bypassing feedback mechanisms in antibody production. Many people who suffer from autoimmune diseases have a genetic predisposition and environmental factors can trigger the production of autoantibodies.
Autoimmune diseases often have inflammatory effects where autoantibodies initiate immune system activation against a particular cell type or a subset of cell types.
For example, in type I diabetes, antibodies that act against pancreatic beta cells are produced, ultimately leading to beta-cell destruction and loss of insulin production.
Anti-NMDAR encephalitis
The N-methyl-D-aspartate receptor (NMDAR) is a glutamate receptor found in different types of nerve cells. The flow of Ca2+ through the receptor, activated by glutamate binding, is thought to be key in learning and memory.
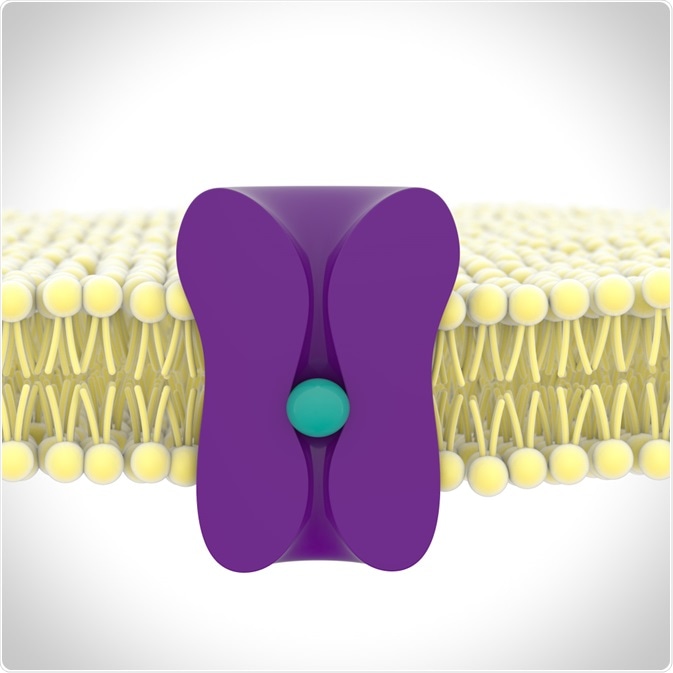
Image Credit: sonorileto/Shutterstock.com
Anti-NMDAR encephalitis is characterized by inflammation of the brain caused by autoantibodies. In women, this is often induced by the presence of a tumor, particularly an ovarian teratoma. Other causes include the herpes simplex virus.
IgG anti-NMDAR antibodies bind the GluN1 subunit of the NMDAR heterotetramer, removing it from the synapse. This often results in psychiatric problems for the patient, including the development of psychosis, and it is likely to have an important role in schizophrenia.
Further to this, a study in China demonstrates a correlation between the concentration of anti-NMDAR antibodies and the severity of psychiatric symptoms. Patients with a higher titer of antibodies are more likely to display psychiatric symptoms as the initial symptom of the disease.
Antibodies aren’t capable of passing across an intact blood-brain barrier. The presence of anti-NMDAR antibodies in the brain is likely due to a compromised blood-brain barrier, commonly caused by tumors or chronic stress. Another mechanism could be the direct secretion of antibodies into the central nervous system by B cells.
This allows the antibodies to accumulate in brain tissue at a high enough concentration to eventually lead to the onset of anti-NMDAR encephalitis and psychiatric symptoms.
Beneficial effects of anti-NMDAR antibodies
Researchers at the Max Planck Institute of Experimental Medicine in Göttingen found that anti-NMDAR antibodies can have an anti-depressive effect under the right conditions, showing reduced levels of anxiety and depression in certain individuals.
Previous studies had shown an increase in seroprevalence with age. However, this age dependence was not shown in some individuals, including refugees and migrants, indicating a possible link between chronic stress early in life and the formation of anti-NMDAR antibodies.
The high seroprevalence in young refugees could be seen to be dangerous. If they were to suffer a loss of integrity to the blood-brain barrier, the autoantibodies could flood into the brain tissue and cause severe psychiatric disease, including epileptic seizures.
However, this also indicates the potential for these antibodies to have a function in relieving stress. To test this hypothesis, the researchers compared the effect of anti-NMDAR antibodies on healthy mice to those with an impaired blood-brain barrier, both of which were exposed to chronic stress.
Depressive behavior was less prevalent in mice with an impaired blood-brain barrier, where anti-NMDAR antibodies were able to accumulate in the brain tissue. This indicates a potential anti-depressive role of these antibodies.
Hannelore Ehrenreich, a lead researcher on the project, commented on the differing effects of anti-NMDAR antibodies, stating: “the effect of these autoantibodies […] is determined not only by their level in the brain but also by any underlying condition, in particular the presence or absence of inflammation.”
Conclusion
Further research is required on the exact mechanism of the anti-NMDAR antibody function. Significant variations in seroprevalence and outcome, whether anti-depressive or onset of encephalitis, indicate a strong role of environmental factors in antibody activity.
This may be key to developing our understanding of the mechanisms underlying various psychiatric diseases, caused by the onset of anti-NMDAR encephalitis. It may also contribute to the development of novel treatments, helping patients to manage their symptoms and take steps towards improved mental health.
It will also provide insight into how the body copes with situations of extreme mental stress, such as those for refugees and asylum seekers. Researching the seroprevalence of anti-NMDAR antibodies in individuals experiencing different types of chronic stress may help to further understand their function.
These antibodies appear to play a similar role in the brain to the anti-depressant ketamine, which also acts on the NMDA receptor. An anti-depressive mechanism for ketamine has been proposed, which could act as a potential model for understanding the mechanism by which anti-NMDAR antibodies relieve depressive symptoms.
References
- Hammer, C. et al. (2014) ‘Neuropsychiatric disease relevance of circulating anti-NMDA receptor autoantibodies depends on blood-brain barrier integrity’, Molecular Psychiatry. Nature Publishing Group, 19(10), pp. 1143–1149. doi: 10.1038/mp.2013.110.
- Kayser, M. S. and Dalmau, J. (2016) ‘Anti-NMDA receptor encephalitis, autoimmunity, and psychosis’, Schizophrenia Research. Elsevier B.V., pp. 36–40. doi: 10.1016/j.schres.2014.10.007.
- Pan, H. et al. (2020) ‘Multiple inducers and novel roles of autoantibodies against the obligatory NMDAR subunit NR1: a translational study from chronic life stress to brain injury’, Molecular Psychiatry. Springer Nature, pp. 1–12. doi: 10.1038/s41380-020-0672-1.
- Wang, W. et al. (2020) ‘Psychiatric Symptoms of Patients With Anti-NMDA Receptor Encephalitis’, Frontiers in Neurology. Frontiers Media S.A., 10. doi: 10.3389/fneur.2019.01330.
- www.mpg.de (2020) Antibodies: the body’s own antidepressants | Max-Planck-Gesellschaft. Available at: https://www.mpg.de/14495085/nmda-recptor-autoantibodies-antidepressants (Accessed: 22 March 2020).
Further Reading
Last Updated: Apr 17, 2020