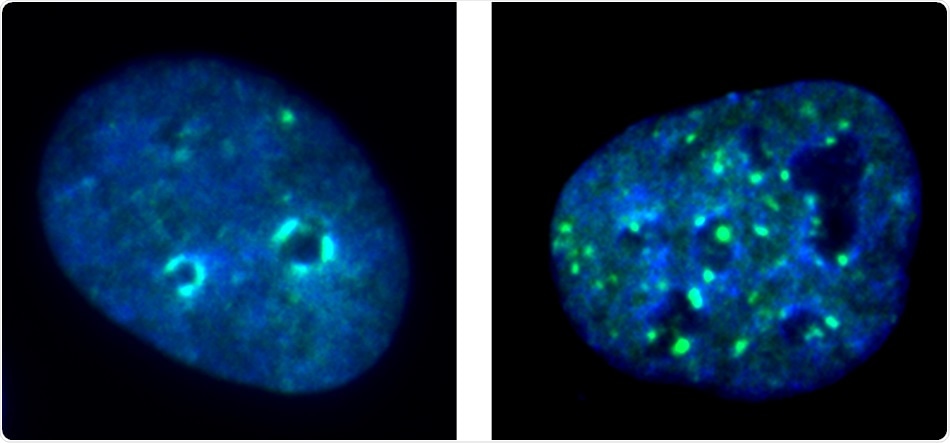
Immunofluorescence images show the nucleus of a cancer cell with KDM4A (left) and a cancer cell nucleus after KDM4A is removed (right), with DNA-protein condensate dots in green. Image Credit: UCLA School of Dentistry.
The researchers achieved this feat by focusing on an enzyme that plays a crucial role in head and neck cancer cells.
Immunotherapy is used as a clinical treatment for different types of cancers. This therapy harnesses the natural defenses of the body to combat the disease. But certain cancers, such as head and neck squamous cell carcinomas, do not respond well to immunotherapy as other types of cancers do. For such neck and head cancers, the prognosis is poor and has a high mortality rate of five-years; hence, effective treatments for such cancers are urgently needed.
The UCLA researchers, headed by distinguished professor Dr. Cun-Yu Wang, chair of oral biology at the dentistry school, revealed that by focusing on susceptibility in the cellular process of tumor immunity and duplication, they could influence the response of tumor cells to immunotherapy.
The team targeted the KDM4A enzyme, the so-called epigenetic factor. This molecule controls the expression of genes, silencing certain genes in cells and triggering others. Overexpression of the KDM4A enzyme in squamous cell neck and head cancers supports gene expression associated with the replication and metastasis of cancer cells.
Tumor cells are known to spread considerably, evading the immune system, and they can metastasize to other parts of the body, including lymph nodes, if not monitored. In this case, when cancer cells that grow in the epithelial layer—lining the structures of the neck and head—can transform into head and neck squamous cell carcinoma when unchecked.
Cancer cells replicate via the abnormal spread and stimulation of signaling pathways for tumor cells, and the team speculated if they could potentially disturb these processes and identify susceptibility and whether it is possible to alter the body’s response to fight cancer cells and its reaction to external immunotherapy.
We know that the KDM4A gene plays a critical role in cancer cell replication and spread, so we focused our study on removing this gene to see if we would get an opposite response.”
Dr Cun-Yu Wang, Study Corresponding Author and Member, UCLA Jonsson Comprehensive Cancer Center
By eliminating the KDM4A gene from the mouse models, the investigators observed a significant reduction in squamous cell carcinomas and relatively less metastasis of cancer cells to the lymph nodes, which are precursors to the proliferation of the disease throughout the body.
Unexpectedly, the researchers also found that the removal of the KDM4A gene resulted in the recruitment and stimulation of the body’s infection-fighting T cells, which destroyed cancer cells and activated the innate tumor immunity.
The researchers subsequently tried to figure out why the squamous carcinoma cells had such a poor reaction to immunotherapy. They used another set of mouse models, once again removed the KDM4A gene, and added a PD-1 blockade, which signals immunotherapy medications to attack the tumor cells.
The combination of KDM4A removal and immunotherapy further reduced the growth of squamous cell cancer and the metastasis of the lymph nodes.
The team also wanted to find out if a small-molecule inhibitor of the KDM4A gene could boost the effectiveness of the original immunotherapy based on the PD-1 blockade. They observed that this inhibitor also considerably helped eliminate cancer stem cells, which are linked to cancer relapse.
The results could lead to the development of more specific inhibitors for the KDM4A gene as well as more effective immunotherapies for cancer.
I am continuously impressed by Dr. Cun-Yu Wang and his team for breaking through barriers in our understanding of cancer-causing cellular processes. The results of this study have major implications for the development of more effective, life-saving cancer therapies.”
Dr Paul Krebsbach, Dean and Professor, UCLA School of Dentistry
Source:
Journal reference:
Zhang, W., et al. (2021) Targeting KDM4A epigenetically activates tumor-cell-intrinsic immunity by inducing DNA replication stress. Molecular Cell. doi.org/10.1016/j.molcel.2021.02.038.