 By Pooja Toshniwal PahariaReviewed by Lexie CornerJun 20 2025
By Pooja Toshniwal PahariaReviewed by Lexie CornerJun 20 2025A recent study published in Nature Genetics investigated the genetic factors that enable Shigella flexneri to colonize the human gut. The researchers focused on identifying specific genes required for colonizing human intestinal epithelial cells (IECs).
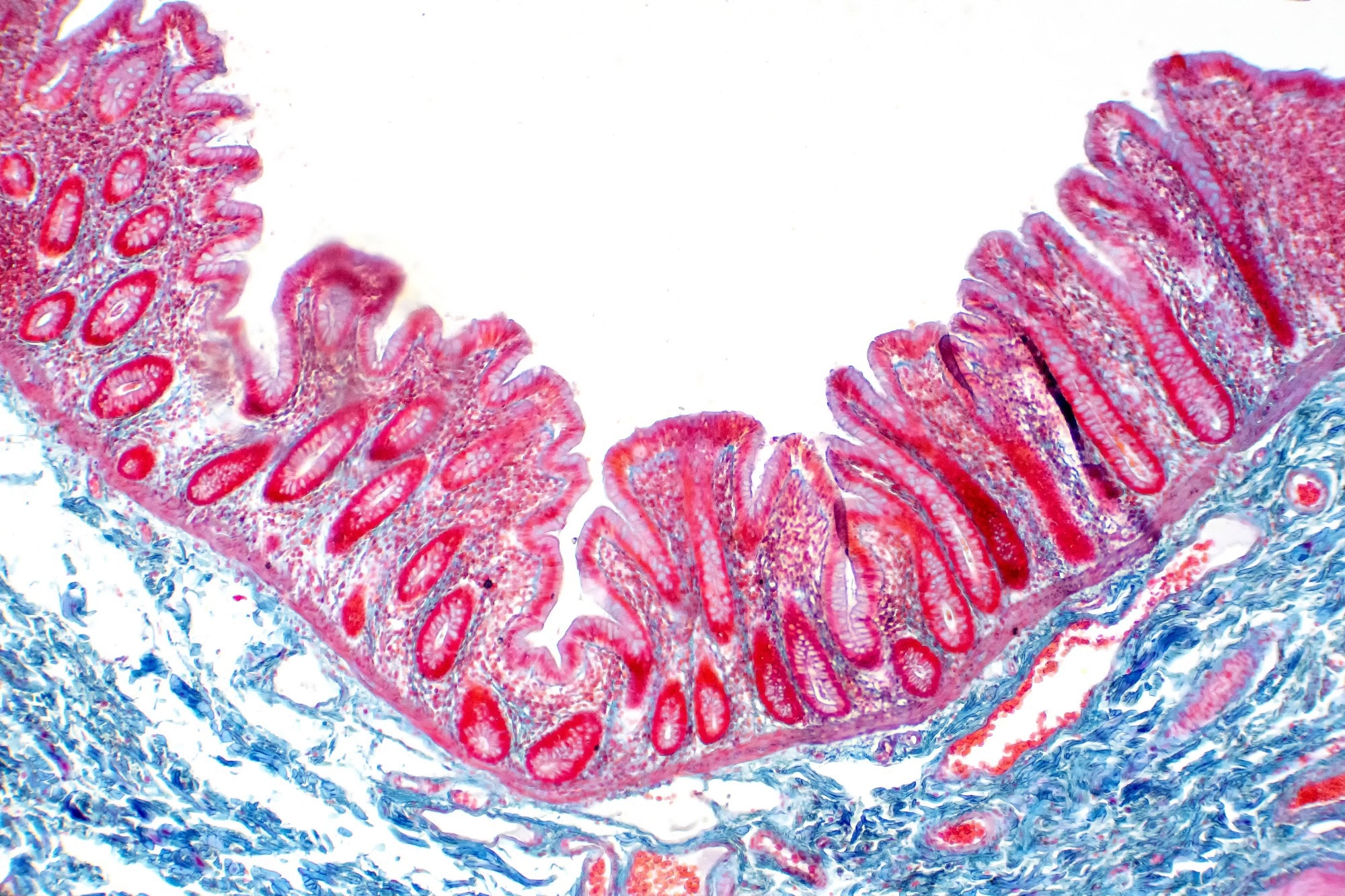 Image Credit: Choksawatdikorn/Shutterstock.com
Image Credit: Choksawatdikorn/Shutterstock.com
They developed a scalable gut epithelial organoid model to map the genome-wide colonization landscape of S. flexneri. The study highlighted the key role of type III secretion system (T3SS) effectors in Shigella virulence. Inhibiting these effectors may reduce the bacterium’s ability to colonize the gut and cause disease, making them potential targets for future therapies.
S. flexneri, a Gram-negative pathogen, is a known cause of bacillary dysentery in humans and primates. However, animal models do not fully replicate human gut physiology, which limits their use in studying Shigella pathogenesis. Commonly used tumor-derived cell lines also show altered characteristics, which can distort observations of bacterial invasion.
As a result, the genetic mechanisms that govern Shigella colonization of the gut epithelium remain unclear. Organotypic tissue culture models offer a promising approach to study these host-microbe interactions.
About the Study
The researchers developed a gut epithelial model to explore the genetic basis of S. flexneri infection. They used resected jejunal and non-tumor colon tissue to generate three-dimensional enteroids and colonoids.
They established gentamicin-protected enteroid cultures with basal-out (BO) polarity. Immunostaining and confocal microscopy enabled the analysis of enteroid morphology following infection with the wild-type S. flexneri M90T strain.
To identify genes important for colonization, the team created Tn5 transposon mutant libraries. They combined 43 sub-libraries—each with 10,000 to 30,000 mutants—to produce a pool of 130,000 mutants for transposon-directed insertion sequencing (TraDIS).
TraDIS linked gene disruptions to bacterial fitness. RNA sequencing was used to relate fitness to expression of T3SS virulence genes. This integration allowed estimation of the genetic expression cost of virulence.
They validated these findings using barcoded consortium infection assays. Each assay exposed 800 enteroids to mutant sub-libraries alongside wild-type strains. After six hours, the team collected 40,000 to 200,000 bacterial cells per infection. Inoculum (input) and intracellular (output) bacteria were then enriched at 30 °C or 37 °C to examine how temperature affects bacterial growth.
Mass spectrometry-based proteomics was used for protein profiling. Simulations of the output mutant library revealed a bottleneck of roughly 2,000 bacteria during infection, indicating strong selection pressure.
To maintain statistical power while managing this bottleneck, the team conducted 40 infections using 2,000–3,000 mutants each. Bayesian modeling with a zero-inflated negative binomial (ZINB) distribution helped extract reliable fitness estimates despite random loss of certain strains.
Results
The study found that S. flexneri relies on four T3SS effectors during early colonization of intestinal epithelial cells: IpgB1, IpgB2, IpaA, and VirA. IpgB1 and IpgB2 induce actin ruffling, aiding initial attachment. IpaA helps with actin depolymerization, facilitating invasion from the intestinal and colonic sides. VirA, a Rab inhibitor, also contributes to colonization. Notably, the role of IpaA varied depending on the specific intestinal region and cell environment.
The team identified 105 genes that support Shigella invasion of enteroids. These included the virF and virB transcriptional regulators, the RpoS sigma factor, IraM anti-adapter protein, and polyribonucleotide phosphorylase (PNPase). Additional contributors included FabF (involved in fatty acid synthesis) and genes related to sulfur metabolism.
Mutants lacking virB and virF showed increased growth at 37 °C, suggesting that loss of T3SS regulation benefits bacterial growth. However, disrupting individual T3SS effectors had minimal fitness costs. Mutants such as ΔtolC, ΔacrA, ΔacrB, and ΔacrAB—as well as those deficient in O-antigen and lipopolysaccharide (LPS) synthesis—had reduced colonization capacity. This may result from shortened LPS chains, which interfere with proper T3SS docking to the epithelial cell membrane.
The study also found that MnmE and G U34-dependent tRNA modifications affect the T3SS virulence pathway. These modifications enhance translational accuracy, particularly at codons ending in A or G, and thereby support the production of key virulence proteins.
Proteomic analysis showed reduced expression of proteins such as virB and other T3SS components. These proteins had high usage of the AGA codon, whose corresponding tRNA is modified by MnmE/G. This finding may explain the reduced colonization efficiency in mutant strains lacking these modifications.
Download your PDF copy now!
Conclusion
The study demonstrated that Shigella flexneri colonization of the human gut depends on specific genetic factors, particularly T3SS effectors. Using a human-derived organotypic model, the researchers identified key genes and mechanisms that influence bacterial invasion and survival.
Their work provides a foundation for future functional genomics research in complex infection models. The organoid-based approach used here can be adapted for genome-wide screening of other pathogens and across varied infection conditions and time scales.
Journal Reference
Di Martino, M.L., et al. (2025). A scalable gut epithelial organoid model reveals the genome-wide colonization landscape of a human-adapted pathogen. Nat Genet., DOI: 10.1038/s41588-025-02218-x, https://www.nature.com/articles/s41588-025-02218-x