Reviewed by Lauren HardakerSep 29 2025
The yeast fungus Candida albicans employs the toxin candidalysin not only to cause infections but also to inconspicuously colonize the oral mucosa, though only in precisely regulated amounts. Insufficient toxin levels hinder oral colonization, while excessive amounts activate the immune system and trigger an inflammatory defense response, as revealed by an international research team from Zurich, Jena, and Paris. Their findings were published in Nature Microbiology.
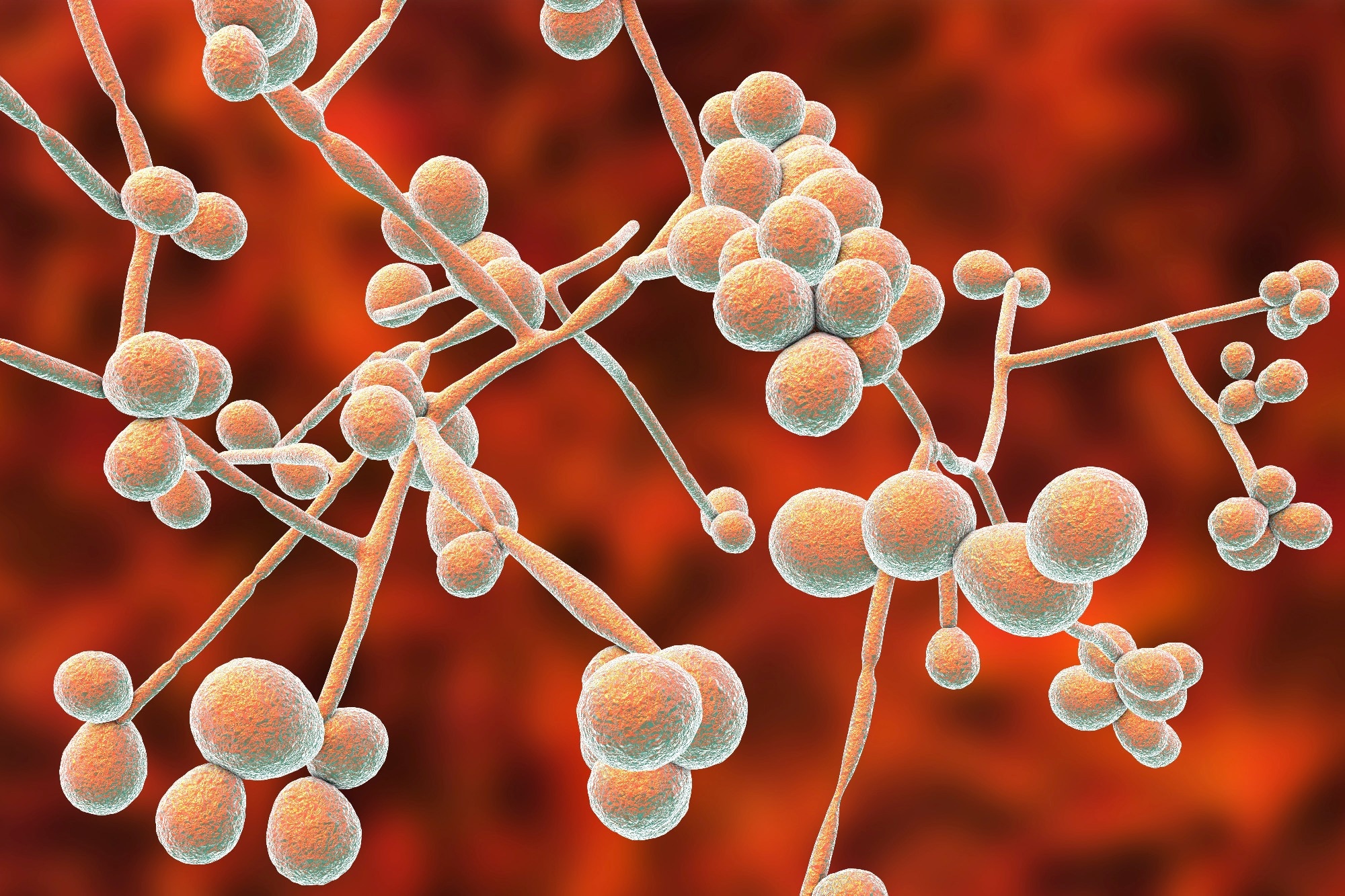 Image credit: Kateryna Kon/Shutterstock.com
Image credit: Kateryna Kon/Shutterstock.com
Candida albicans naturally resides in the human microbiome and is typically harmless. Under certain conditions, however, it can shift from its round yeast form to a filamentous, hyphal state and cause infections that may be life-threatening, particularly in immunocompromised individuals. In this hyphal form, C. albicans produces the toxin candidalysin, a protein that directly damages host cells.
We knew that the fungal toxin candidalysin can cause disease. What is new is that it is also necessary for the fungus to survive in the mouth. The yeast fungus Candida albicans uses the toxin like a door opener to anchor itself in the mucous membrane. As long as it only produces it in small quantities, it remains under the radar of the immune system and survives in the oral cavity in the long term.
Bernhard Hube, Head, Department of Microbial Pathogenicity Mechanisms, Leibniz Institut for Natural Product Research and Infection Biology (Leibniz-HKI)
Bernhard Hube is also the Chair of Microbial Pathogenicity at Friedrich Schiller University in Jena.
A global team used mouse models to clarify this connection. Researchers, under the leadership of Salomé LeibundGut-Landmann at the University of Zurich, demonstrated the immune system's response to various fungal strains to explain this relationship. The Leibniz-HKI in Jena provided insights into the genetic foundations: the team employed targeted interventions to alter genes responsible for hyphae formation and toxin synthesis in the yeast fungus. Subsequently, researchers at the Institut Pasteur in Paris conducted bioinformatic analyses to position the genetic data within an evolutionary framework.
Two distinct strains of Candida were compared: The aggressive laboratory strain SC5314 is known for forming elongated hyphae and generating significant quantities of candidalysin. Consequently, the immune system responds promptly with intense inflammation, rapidly eliminating the fungus. In contrast, strain 101, which is found naturally in the oral cavity, exhibits a markedly different behavior: it produces minimal amounts of the toxin, allowing it to remain unnoticed within the mucous membrane without provoking a robust immune reaction.
“The fungus drives with the handbrake on, so to speak. It needs a little toxin, but too much is immediately punished,” said Hube.
It is precisely these differences between the strains that show how important the fine regulation of candidalysin is for colonizing different niches in the body. Only if Candida albicans finds the correct amount, then the fungus can survive in the mouth long-term without being fought by the immune system.
Tim Schille, Doctoral Researcher, Leibniz-HKI
The EED1 gene is also crucial in this process. It governs the formation of hyphae and consequently indirectly affects the production of candidalysin. This enables the fungus to stay mostly undetected within the oral mucosa. Nevertheless, if this equilibrium is disturbed, infections may arise.
It is remarkable how well the fungus regulates its activity. This balance also explains why the toxin has been preserved evolutionarily: it enables the fungus to live permanently in the oral mucosa, but at the same time makes it dangerous as a potential pathogen.
Tim Schille, Doctoral Researcher, Leibniz-HKI
The study indicates that candidalysin could play a significant role in Candida yeasts' colonization of specific regions of the body. To date, the findings have only provided provisional possibilities for medical applications.
“We cannot yet derive any therapeutic applications for oral Candida infections. In the case of vaginal infections, however, we have already been able to show in earlier studies that the toxin can be neutralized. This can significantly reduce tissue damage caused by Candida albicans, which is typical of vaginal yeast infections,” said Hube.
Source:
Journal reference:
Fróis-Martins, R., et al. (2025). Dynamic expression of candidalysin facilitates oral colonization of Candida albicans in mice. Nature Microbiology. doi.org/10.1038/s41564-025-02122-4.