 By Pooja Toshniwal PahariaReviewed by Lauren HardakerJul 30 2025
By Pooja Toshniwal PahariaReviewed by Lauren HardakerJul 30 2025In a recent study published in Frontiers in Immunology, researchers investigated transglutaminase-2 (TG2) inhibition as a therapeutic strategy for ovarian malignancies. They found that TG2 inhibition and genetic deletion of TG2 recalibrate the immune system to mount a stronger anti-tumor response, offering a new avenue for developing targeted treatments for this aggressive cancer. The strongest immune effects were observed in mice lacking TG2, where the absence of TG2 increased natural killer (NK), B, and T cells, while reducing immunosuppressive tissue-associated macrophages (TAMs) to slow down the metastatic progression of tumors.
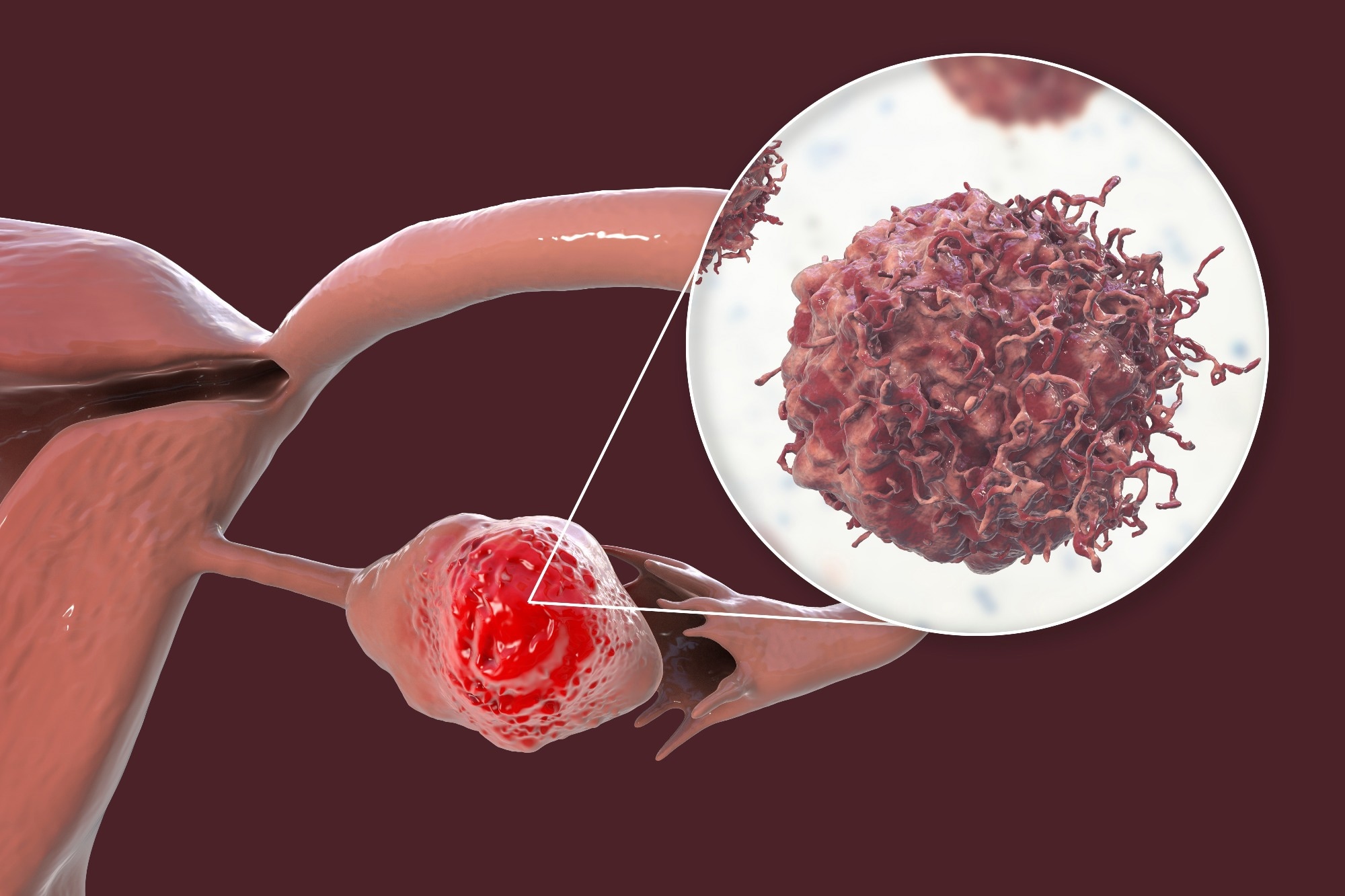 Image credit: Kateryna Kon/Shutterstock.com
Image credit: Kateryna Kon/Shutterstock.com
Ovarian cancers are fatal gynecological malignancies with poor five-year survival rates. The intercellular complexities of the tumor microenvironment (TME) might lead to immunosuppression and chemoresistance, challenging treatment efficacy. Understanding the molecular interrelationships within the TME is essential when designing novel therapeutic options.
TG2, a protein involved in various pathophysiological and biological processes, promotes ovarian cancer progression by potentiating peritoneal disease and enhancing tumor cell dissemination. The protein also alters immunological composition and function toward a more immunosuppressive phenotype, reducing the ability to fight tumors.
About the Study
The present study researchers explored whether novel small-molecule transglutaminase-2 inhibitors could improve ovarian cancer outcomes.
The team performed ribonucleic acid (RNA) sequencing, immunohistochemistry, and flow cytometry to investigate TG2 actions in ovarian cancers. They analyzed the therapeutic effects of several TG2 inhibitor molecules (AA9, NC9, NF20, JA38, and VA4) in OV1946 and SKOV3 ovarian cancer xenograft models.
Quantitative polymerase chain reaction (qPCR) and western blot analysis identified cells expressing TG2 (OV1946, OVCA420, TOV3041G, and SKOV3). To assess the effects of TG2 inhibitors on cell survival, the researchers injected SKOV3 (low TG2 expression) and OV1946 (high TG2 expression) cancer cells intraperitoneally into NOD scid gamma (NSG) mice. Subsequently, the mice received DMSO vehicle control, NC9 (20 mg/kg), or VA4 (20 mg/kg) treatment.
Further, the team investigated whether the effects of TG2 inhibition on ovarian cancer cells involve epithelial-mesenchymal transition (EMT). Transforming Growth Factor-beta 1 (TGF-β1) treatment induced EMT in the ovarian cancer cells to determine the association between TG2 and EMT by profiling EMT genes such as cadherin 2 (CDH2), vimentin (VIM), and snail family transcriptional repressor 1 (SNAI1).
Researchers injected metastatic ID8 cells lacking the transformation-related protein 53 (Trp53-/-) and breast cancer gene-1 (Brca1-/-) or non-metastasizing KPCA cells into mice to determine the role of TG2 in metastasis and immune composition. They analyzed differences in disease progression six weeks post-injection and compared the immune composition of TRP53- and BRCA1-negative ID8 tumors with and without TG2 in the tumor microenvironment. These ID8 tumors underwent RNA sequencing after six weeks of intrabursal injections to reveal the transcriptional changes involved in retarding tumor progression in the TGM2 knockout murine model.
Results
TG2 inhibitors did not significantly affect cell proliferation or migration in ovarian cancer cell lines; however, they decreased the invasive capacity of these cells. The inhibition of TG2's transamidation catalytic and guanosine triphosphate (GTP) binding activities is crucial for reducing invasiveness. Specifically, the TG2 inhibitor VA4 prolonged survival by 22% in SKOV3 tumor-bearing mice, although the effect was modest (median days of survival, 39 days vs. 32 days in the DMSO vehicle control). No survival benefit was seen in OV1946-bearing mice treated with TG2 inhibitors, indicating a limited therapeutic effect in this model.
An extended survival in TG2 absence resulted from delayed metastatic dissemination in ID8 cells, devoid of two tumor suppressor genes, TRP53 and BRCA-1. Tumor-bearing Brca1-/- and Trp53-/- mice without TG2 demonstrated a median survival of 111 days (vs. 56 days in wild-type mice). However, TG2 inhibition did not alter the survival rates of non-metastatic cells. Since TG2 expression varies within human ovarian cancer cells and its impact on survival differs between metastatic and non-metastatic models, TG2 expression could potentially be considered a biomarker to help identify patients most likely to benefit from TG2-targeted therapies, moving towards more personalized treatment strategies.
TG2 inhibition reduced the immunosuppressing tumor-associated macrophage (TAM) counts while increasing B cell activation and NK and CD8+ T cell frequencies primarily in TG2-deficient mice rather than through direct drug effects. RNA sequencing revealed that the deficiency of TG2 proteins in the tumor microenvironment enriched pathways associated with B cell stimulation and regulation, underscoring that B cell activity is central to the survival benefit.
However, TG2 inhibition did not affect EMT gene expression or macrophage polarization in vitro. The findings suggest that TG2 inhibition, and more strongly TG2 loss, could be a strategy to 're-educate' the immunological system to fight cancer better.
Conclusions
The study findings indicate that TG2 inhibitors reduce tumor invasiveness and may prolong survival by delaying metastasis. However, their most significant therapeutic implications come from insights into how TG2 deletion reshaped the TME, particularly through B cell regulation and immune activation. TG2 targeting could be a promising strategy to improve anti-tumoral responses in ovarian malignancies, particularly by influencing the function of B cells.
Further investigation into TG2's role in B cell functions could lead to new therapeutic opportunities. For instance, TG2 inhibitors could enhance the effectiveness of immunotherapies that rely on or benefit from a robust B cell response. TG2 inhibition may improve outcomes for patients who respond poorly to current immune checkpoint inhibitors.
Journal reference
Ibrahim D. et al. (2025). Transglutaminase 2 regulates ovarian cancer metastasis by modulating the immune microenvironment. Front. Immunol., 16:1639853. DOI: 10.3389/fimmu.2025.1639853 https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1639853/full