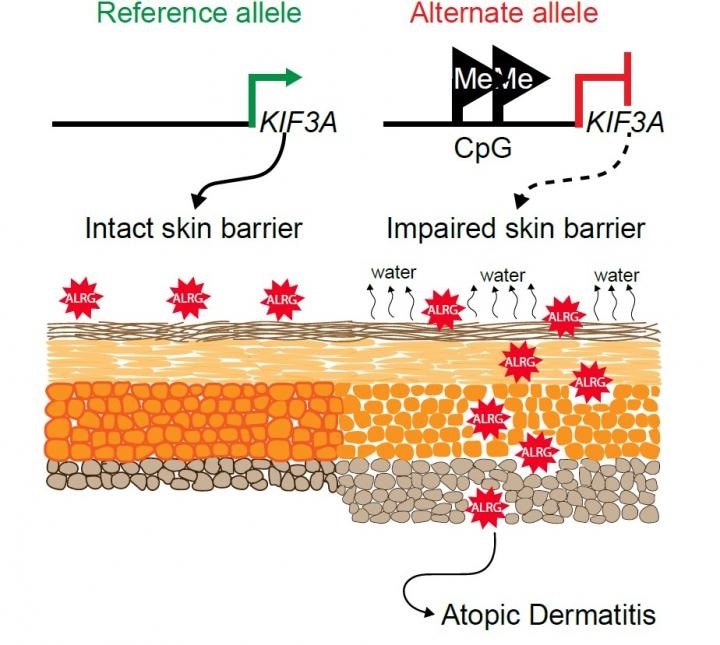
This graphical abstract shows how two variations in the gene KIF3A can disrupt the skin barrier, allowing allergens to penetrate into deeper layers. Image Credit: Cincinnati Children’s Hospital Medical Center.
This condition would consequently enable environmental exposures to more easily penetrate the skin barrier and play a role in the development of asthma and food allergies as the children grow up.
Mariana Stevens, PhD, is the study’s first author, and Gurjit Khurana Hershey, MD, PhD, Director, Division of Asthma Research, is the senior corresponding author.
The study offers new insights into the molecular and genetic mechanisms involved in atopic dermatitis, also called eczema—a common condition that affects 20% of all children. While this skin condition usually resolves as kids age, several children with disrupted skin barriers continue to develop food allergies and asthma, which are more severe conditions.
The study results could make it relatively simpler to find out which group of children with eczema is most likely to develop other allergic conditions. This strategy would enable many preventive therapies, including lifestyle interventions, to be targeted toward children who have a higher risk. The latest research also implies a novel target for promising treatment.
Food allergies are rising and the causes are not entirely clear. This study adds evidence to a rising theory that skin health is more closely connected to lung and gut health than many have suspected.”
Gurjit Khurana Hershey, MD, PhD, Director, Division of Asthma Research, Cincinnati Children’s Hospital Medical Center
Two tiny SNPs play big roles in skin health
A common genetic variation in a DNA sequence is a single nucleotide polymorphism, or SNP. In this work, the team observed that two SNPs in the KIF3A gene—validated via a range of experiments in children and also through preclinical studies conducted in mice—play direct roles in the development of eczema.
The rs2299007 and rs11740584 SNPs are associated with an increased loss of water via the skin, dry skin, and the typical damage observed in atopic dermatitis. Quantifying the speed of this kind of water loss is one approach to determine the level of eczema severity in a child.
The KIF3A gene should function properly because it helps cells create their primary cilia, which is a structure found on the surfaces of cells and serves as an antenna to receive significant signal data from other kinds of cells.
Earlier studies, headed by scientists from Cincinnati Children’s Hospital Medical Center and others, have already demonstrated that a malfunctioning KIF3A gene in lung tissue can cause asthma. Similarly, malfunctions of the same KIF3A gene in the gut tissues can raise the risk of food allergies.
Now, this latest research helps link both these allergy risks to an impaired skin barrier, which allows more allergy-activating substances to enter inside the human body to trigger immune system over-reactions.
We are working to better understand how skin, gut and lung health are connected. In fact, we have a grant from the National Institutes of Health to further study this connection.”
Gurjit Khurana Hershey, MD, PhD, Director, Division of Asthma Research, Cincinnati Children’s Hospital Medical Center
Development underway for screening test
At the Cincinnati Children’s Hospital Medical Center, the researchers have started to look for drug compounds that might help restore the disrupted functions of the KIF3A gene in the near future. However, the first subsequent step based on this research will be to continue an ongoing quest for a fast screening test.
The novel study is based on discoveries from two other research works published earlier in 2020 by scientists from Cincinnati Children’s Hospital Medical Center.
- In February 2020, a study published in the Journal of Allergy and Clinical Immunology reported that the risk of allergy posed by atopic dermatitis was higher than having a single parent with allergic disease.
- Then in April 2020, a study published in the same journal showed the value of applying pain-free tape stripping as a less-invasive tool when compared to skin biopsies for collecting information about skin health.
According to Hershey, the aim is to apply skin tape strip samples to measure the expression of the KIF3A gene as a promising tool for estimating disease risk.
The team is analyzing this method in a group of 600 children from the Cincinnati area who were identified with atopic dermatitis early in their life. This group of children, the first cohort of its kind in the United States, will be tracked for five years to directly assess the potential of KIF3A genetic differences and skin expression to estimate disease risk.
Source:
Journal reference:
Stevens, M. L., et al. (2020) Disease-associated KIF3A variants alter gene methylation and expression impacting skin barrier and atopic dermatitis risk. Nature Communications. doi.org/10.1038/s41467-020-17895-x.