 By Pooja Toshniwal PahariaReviewed by Lauren HardakerJul 3 2025
By Pooja Toshniwal PahariaReviewed by Lauren HardakerJul 3 2025In a recent study published in Advanced Healthcare Materials, researchers engineered an animal-free macrophage-adipocyte co-culture model to investigate adipose tissue inflammation. The human cell-derived model demonstrates the macrophage-adipocyte crosstalk in health and disease in vitro by replicating the intercellular dynamics in adipose tissues. The model can improve understanding of inflammation-related metabolic diseases, such as obesity. Additionally, scientists can use the inflamed macrophage-adipocyte co-cultures to test anti-inflammatory treatment strategies and incorporate patient-derived cell material for personalized medicine approaches.
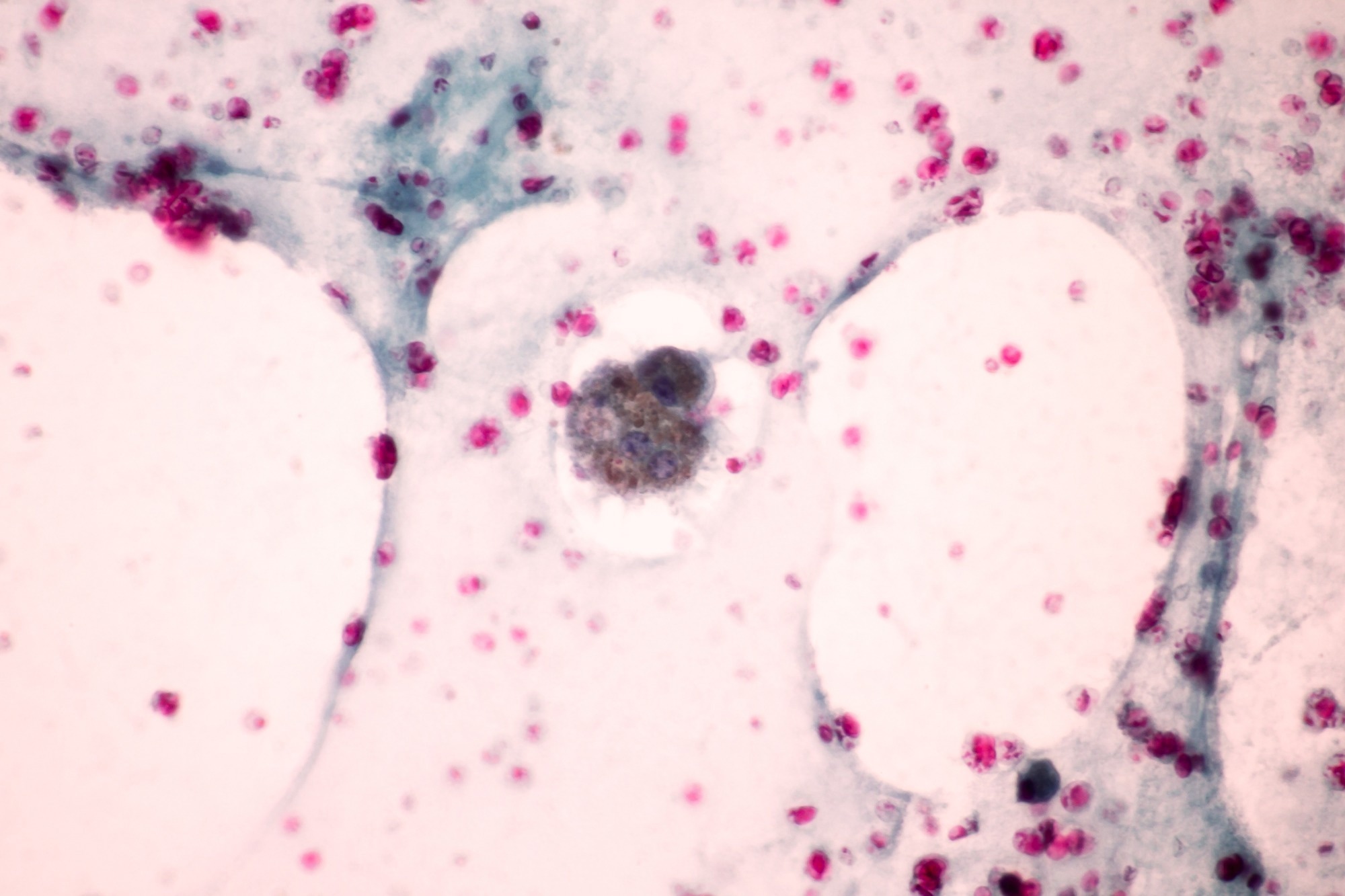 Image credit: Komsan Loonprom/Shutterstock.com
Image credit: Komsan Loonprom/Shutterstock.com
Inflammation of the adipose tissue is crucial for the development of metabolic diseases, characterized by the secretion of inflammatory cytokine molecules and infiltration of immune cells, especially macrophages. Depending on their activation state, macrophages can adopt either pro-inflammatory or anti-inflammatory roles, influencing tissue health or dysfunction.
While animal models have been frequently used to unravel mechanisms underlying adipose tissue dysregulation, physiological differences in the adipose tissues across species limit the transferability of findings to humans. There is a growing need for in vitro testing systems that accurately replicate the environment of inflamed adipose tissues. These systems should ideally not contain animal-based components, such as collagen, to avoid variability and ethical concerns associated with serum and other animal products.
About the study
In the present study, researchers developed a human adipocyte-macrophage model as an alternative to animal models for preclinical research testing.
The researchers obtained mature adipocytes (ACs) from human subcutaneous white adipose tissue biopsy samples. They co-cultured two human acute monocytic leukemia cell lines, Tohoku Hospital Pediatrics-1 (THP-1) and Mono Mac (MM6), with ACs in 0.5% gellan gum (GG) hydrogels, a synthetic, animal-free extracellular matrix substitute. They compared GG with collagen to verify GG's suitability as a matrix material. Assessment parameters included viability, intracellular lipid levels, and the integrity of lipid vacuoles in the adipocytes.
The team used gram-negative bacteria-derived lipopolysaccharide (LPS) and phorbol 12-myristate 13-acetate (PMA) to activate the cell lines and simulate an acute, inflammation-like state in the adipose environment, reflecting characteristics of obesity-related inflammation. Researchers performed clumping phenotypic assays and viability testing in the PMA+LPS condition.
Enzyme-linked immunosorbent assays (ELISA) measured the levels of pro-inflammatory cytokines, such as interleukin (IL)-1ß, 6, 8, and tumor necrosis factor-alpha (TNF-α) in cell culture supernatants over 72 hours of stimulation to quantify immune activation.
Correlating free lactate dehydrogenase (LDH) levels with cell membrane integrity indicated cell turnover and death. Water-soluble tetrazolium (WST) assays were used to analyze metabolic activities. Boron-dipyrromethene (BODIPY) fluorescent staining enabled lipid visualization and quantification in the cells, confirmed by staining the lipid vacuole-coating protein perilipin A. Glycerol (a lipid degradation product) release from the cells indicated their lipolytic activity.
The study also compared individual stimulation with PMA or LPS alone, resulting in lower cytokine secretion than the combined PMA+LPS treatment, highlighting enhanced inflammatory response to the dual-stimulus protocol.
Results
The clumping assay, viability analyses, and inflammatory cytokine quantification tests demonstrated acceptable viability and successful activation of THP-1 and MM6 cells in the defined medium. The activated cells exhibited pro-inflammatory cytokine profiles. The stimulated co-cultures maintained an inflammatory (disease-like) state for three days in the defined medium.
Additionally, intracellular lipids remained abundant in the activated co-cultures. Adipocyte functionality, assessed by perilipin A staining and glycerol release, remained intact in the models. Moreover, the inflamed co-cultures can grow easily in a developed environment, highlighting feasibility and practicality.
The team found GG an appropriate alternative to animal-origin extracellular matrix (ECM) for primary mature adipocytes. Rheological analysis revealed that GG has a gelation point at 8.0 °C, and its viscoelastic moduli remain relatively constant with increasing temperature, unlike collagen, which gels at higher temperatures and exhibits greater stability. GG provided a non-toxic, three-dimensional, ready-to-use, thermosensitive, cross-linking framework of adipose-like tissues, replicating the tissue environment and mechanical properties. GG hydrogels were transparent, non-shrinking, and stable over time, whereas collagen-based hydrogels were opaque and less stable than their clear and non-shrinking GG counterparts. The team found densely packed ACs in GG gels, similar to those in adipose tissue lobules.
The researchers could visualize lipid-comprising cells in GG and collagen matrices a week after culture. The highest LDH release was detected a day after culture using GG hydrogels, normalized until the third day of adipocytes encapsulated in the GG structure. Glycerol concentrations among GG-encapsulated ACs remained similar to those surrounded by collagen. Basal glycerol release increased considerably on day 3, indicating that the activation factors affected lipid metabolism. The co-cultured adipocytes remained viable for three days with abundant lipid-containing vacuoles.
THP-1 cells showed higher overall concentrations of IL-1β compared to MM6. TNF-α secretion in MM6 was comparable between defined and serum-containing media, while stimulated THP-1 cells showed an increasing TNFα pattern over time. IL-6 concentrations in stimulated MM6 were nearly constant, whereas THP-1 cells showed a delayed increase. IL-8 levels were nearly threefold higher in THP-1 than in MM6. The activation levels were generally comparable between serum-containing and defined media but differed between the cell lines, demonstrating cell line-specific inflammatory profiles.
Conclusions
The study findings highlight the development of a three-dimensional co-culture of adipocytes and macrophages for the in vitro study of acute adipose tissue inflammation. The model, comprising mature human ACs in GG hydrogels, promotes cell viability, lipid retention, and pro-inflammatory cytokine secretion.
However, the model is limited to a 72-hour window, reflecting acute rather than chronic inflammation, and does not incorporate other relevant immune or stromal cells, such as T-cells or endothelial cells. The controlled platform offers potential for animal-free preclinical drug testing. Future enhancements, such as incorporating primary human monocytes or extending culture duration, may improve physiological relevance and enable chronic inflammation modelling.
Jornal Reference
S. Now akowski, S. Nellinger, F. B. Albrecht, and P. J. Kluger. (2025). Animal-Free Setup of a 3D Mature Adipocyte-Macrophage Co-Culture to Induce Inflammation In Vitro. Adv. Healthcare Mater., 2500779, DOI: 10.1002/adhm.202500779 https://advanced.onlinelibrary.wiley.com/doi/10.1002/adhm.202500779
Download your PDF copy now!