Reviewed by Lauren HardakerAug 6 2025
Amyotrophic lateral sclerosis (ALS), sometimes known as Lou Gehrig’s disease, is an incurable neurological disease that affects motor neurons, which are nerve cells in the brain and spinal cord that regulate voluntary muscle movement and breathing.
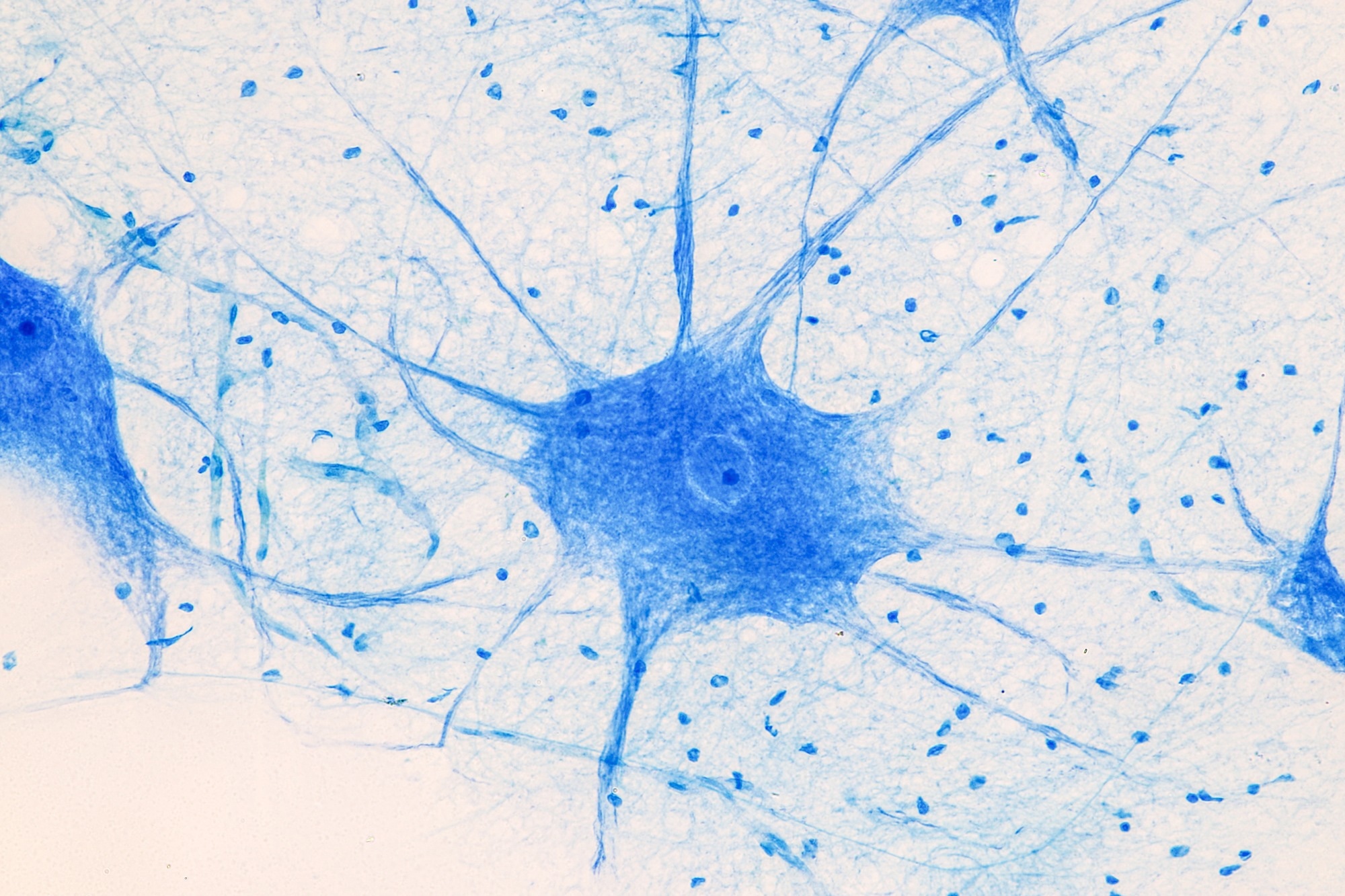 Image credit: Sinhyu Photographer/Shutterstock.com
Image credit: Sinhyu Photographer/Shutterstock.com
Many ALS research studies, particularly those evaluating promising treatments, have failed to meet expectations, often because the severity of the disease varies and people do not all react the same to treatments.
However, a recent study by scientists at Case Western Reserve University employed stem cells derived from ALS patients to target a specific gene as a type of shut-off valve for what strains nerve cells, and it worked.
Although the study featured a relatively uncommon variant of ALS, the researchers were hopeful that the results might give hints for potentially treating the deadly condition more generally.
This work could help lay the foundation for genetically informed clinical trials.
Helen Cristina Miranda, Study Lead Researcher and Associate Professor, Genetics and Genome Sciences, School of Medicine, Case Western Reserve University
Case Western Reserve is particularly strong in regenerative medicine, which involves the generation of healthy cells to replace diseased cells and restore tissues. Miranda’s laboratory uses human stem cells to investigate neurodegenerative diseases like ALS.
The results were published in the peer-reviewed journal EMBO Molecular Medicine.
The Study
The researchers investigated a hereditary form of ALS caused by a gene mutation (vesicle-associated membrane protein B, or VAPB). The VAPB gene encodes instructions for producing a protein that connects various cell regions, allowing them to interact and respond to stress.
Miranda added, “This is especially important in nerve cells. When they break down, the neurons become more vulnerable to degeneration.”
Induced pluripotent stem cells, or iPSCs, are unique cells made in a laboratory from a person’s skin or blood that can differentiate into practically any cell type in the body. This study employed iPSCs from ALS patients to develop motor neurons in a dish, allowing them to examine the condition with actual human cells.
- They observed that a mutation in the VAPB gene can impair communication between important cell components, notably the endoplasmic reticulum (ER) and mitochondria. The ER functions as the cell's quality control center. It aids in protein production and folding and ensures that everything within the cell runs properly, particularly when the cell is stressed. The mitochondria are the cell's power plants. They produce the energy required for cells, particularly nerve cells, to survive and function
- This disturbance triggers the persistent activation of a defensive mechanism known as the Integrated Stress Response (ISR). Although initially beneficial, prolonged ISR activation decreases protein synthesis and cell survival, eventually harming motor neurons and leading to this uncommon hereditary type of ALS
- They also identified ISR as a possible therapeutic target
“We also showed that blocking this stress response can reverse damage in the lab, a promising step toward future treatments. That’s a promising proof-of-concept for future therapeutic strategies,” Miranda stated.
What’s Next
Several drugs authorized for ALS by the US Food and Drug Administration may extend longevity, reduce the rate of deterioration, or assist in controlling symptoms. However, no known medication can stop or reverse the disorder’s course.
As previously stated, the team's study focused on a certain unusual variety of ALS. However, the researchers intend to broaden the study to see if the target can be used to treat different types of the condition.
“It’s very rare, more prevalent in Brazil, but studying it gives us a window into how ALS motor neurons respond to stress. We are now testing ISR inhibitors in more complex neuromuscular models and exploring how this approach might benefit other ALS subtypes,” added Miranda.
Source:
Journal reference:
Landry, C., et al. (2025) Convergent activation of the integrated stress response and ER–mitochondria uncoupling in VAPB-associated ALS. EMBO Molecular Medicine. doi.org/10.1038/s44321-025-00279-3.