To generate a reliable diagnosis, in addition to implementing an effective treatment for all derivatives of cancer, tumor exploration, and imaging is imperative. Today X-Rays, magnetic resonance imaging (MRI’s), and positron emission tomography (PET) scans are the most common apparatus when imaging malignant neoplasms, though new imaging acquisition technologies are being implemented constantly.
Image Credit: Christoph Burgstedt/Shutterstock.com
The two themes most prevalent in tumor imaging are the use of radiopharmaceuticals, (radioisotopes designed for diagnosis & therapy), as well as the diffracting/absorbing properties of these cell masses. Though all tumors are different, each with its own growth rate, differentiation, size, etc., medical experts have formulated criteria to categorize and confront each variant. Tumors are cataloged via their differentiation & anaplasia, their metastasis, their local invasion, and their rate of growth. This will define whether a mass of interest is benign or malignant.
Denoting Differentiation and Anaplasia Using Microscopy
Differentiation and anaplasia especially apply to cells that hold a critical function within their respective organ, tissue, or cell line (parenchyma cells). This parenchyma is made of neoplastic cells, and differentiation refers to their resemblance towards their respective parent cells. In other words, differentiation regards how one neoplastic cell (in the parenchyma) mimic’s its ancestor. This mimicry must be morphological (how similar they look under microscopy), as well as functional (what their role in the body is.)
The greater the differentiation, the more the daughter cell will look like its mother cell. If neoplasms are fully differentiated and are morphologically akin to their progenitor, they are classified as benign. Anaplasia signifies a lack of differentiation and is a hallmark of malignancy. Microscopy recognizes these anaplastic cells by the varied/bizarre shapes of their nuclei, as well as their high nuclear to cytoplasmic ratios.
Denoting Metastasis Using Microscopy
Metastasis is the extent to which cancerous cells spread across the human body. It occurs when masses are cleaved from the original tumor and migrate either through the lymph system or through blood vessels. While some cancers such as liver or ovarian cancer have a lesser amount of secondary tumor sites, other cancers like kidney and breast cancer metastasize at a more elevated rate, spreading to other anatomical sites. This facet of malignancy within a larger area requires MRI and PET methodologies, so that one may obtain a decent image of secondary tumor sites. Though current advances in therapeutics are plentiful, all oncological approaches fall short when combating metastasis, highlighting the importance of these microscopies.
Magnetic Force Microscopy (MRM) in the scope of Functional Magnetic Resonance Imaging (fMRI)
The most familiar field of microscopy that one might associate with cancer is that of “functional magnetic resonance imaging” (fMRI). This would fall under the practice of magnetic force microscopy (MFM), which exposes a target species to magnetic fields. Detection of the resulting electromagnetic signal of said species is what grants us an image, an image reflecting the magnetic resonance of nanoparticles- this offers extremely high resolution.
The nuclei of hydrogen atoms are what the fMRI detects and maps out, elucidating the properties of tissue constructs. For example, oxygenated and de-oxygenated blood differ in biochemical structure. The iron epicenter in hemoglobin can encompass two states of charge, +3 (oxygenated), and +2 (de-oxygenated/reduced). This transition between ions is what allows blood to be oxygenated and deoxygenated.
The fMRI can differ between the different magnetic fields of both charges, allowing us to see levels of unhealthy blood flow and or oxygenation within the brain. The resultant images can indicate many phenotypes like aphasia, ALS, cerebral hypoxia, and other illness related to neural activity.
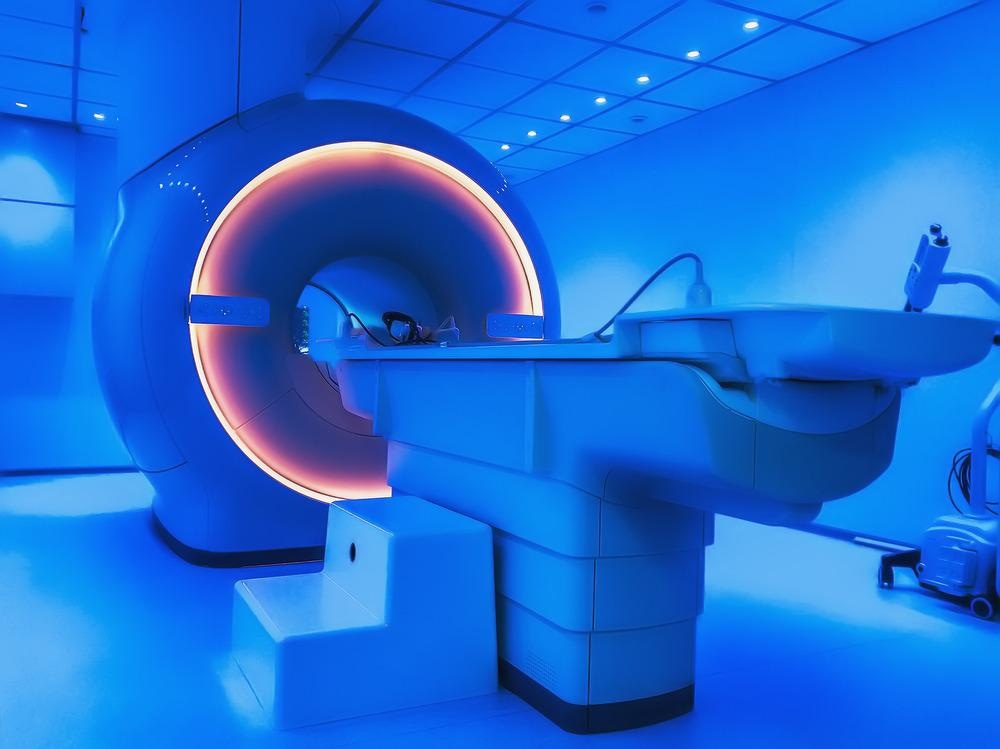
Image Credit: DedMityay/Shutterstock.com
Nano M Slides in In Vitro Assays
Novel instrumentation is always being made to address issues of sample size, one of which are the Nano M slides developed by Abbey B et al. These slides are coated in a thin veneer, while the charged patterned film is sandwiched between the veneer and the glass substrate. The electrons imbued within the patterned film will oscillate when hit with the light of the microscope. This light will pass through the tissue placed atop the veneer and hit the patterned film. The electrons within the patterned film will then change color, solely dependent on the properties of the tissue. In its essence, the charged slide becomes the sensor.
Healthy cells and malignant neoplasms have differing structures and will thus absorb different wavelengths of ambient light. Though the underlining mechanism remains elusive, researchers believe that differences in protein density, cytoskeleton microtubules, or the way cell contents are ordered is what changes the contrast between healthy and cancerous cell lines. Conventional oncology imaging consists of H&E staining (hematoxylin and eosin) followed by light microscopy. However, by circumventing this staining step using these Nano M slides, accuracy is improved, and a great deal of time is saved.
Sources:
- Balaur E, O' Toole S, Spurling AJ, Mann GB, Yeo B, Harvey K, Sadatnajafi C, Hanssen E, Orian J, Nugent KA, Parker BS, Abbey B. Colorimetric histology using plasmonically active microscope slides. Nature. 2021 Oct;598(7879):65-71. doi: 10.1038/s41586-021-03835-2. Epub 2021 Oct 6. PMID: 34616057.
- Kaufmann TJ, Smits M, Boxerman J, Huang R, Barboriak DP, Weller M, Chung C, Tsien C, Brown PD, Shankar L, Galanis E, Gerstner E, van den Bent MJ, Burns TC, Parney IF, Dunn G, Brastianos PK, Lin NU, Wen PY, Ellingson BM. Consensus recommendations for a standardized brain tumor imaging protocol for clinical trials in brain metastases. Neuro Oncol. 2020 Jun 9;22(6):757-772.
- Georgeto, S. M., Zicarelli, C. A., Gariba, M. A., & Aguiar, L. R. (2016). T1-weighted gradient-echo imaging, with and without inversion recovery, in the identification of anatomical structures on the lateral surface of the brain. Radiologia brasileira, 49(6), 382–388.
- Egeblad, M., Nakasone, E. S., & Werb, Z. (2010). Tumors as organs: complex tissues that interface with the entire organism. Developmental cell, 18(6), 884–901.
- Vincent, K., Moore, J., Kennedy, S., & Tracey, I. (2009). Blood oxygenation level-dependent functional magnetic resonance imaging: current and potential uses in obstetrics and gynaecology. BJOG : an international journal of obstetrics and gynaecology, 116(2), 240–246.
- Hong SD, Dhong HJ, Chung SK, Kim HY, Park J, Ha SY. Hematoxylin and eosin staining for detecting biofilms: practical and cost-effective methods for predicting worse outcomes after endoscopic sinus surgery. (2014) Clin Exp Otorhinolaryngol. Sep;7(3):193-7.
Further Reading
Last Updated: Mar 7, 2022