A team of scientists from the Van Andel Institute and the Max Planck Institute for Immunobiology and Epigenetics uncovered two unique subtypes of insulin-producing beta cells, or ß cells, each having important traits that could potentially be used to better understand and treat Type 1 and Type 2 diabetes.
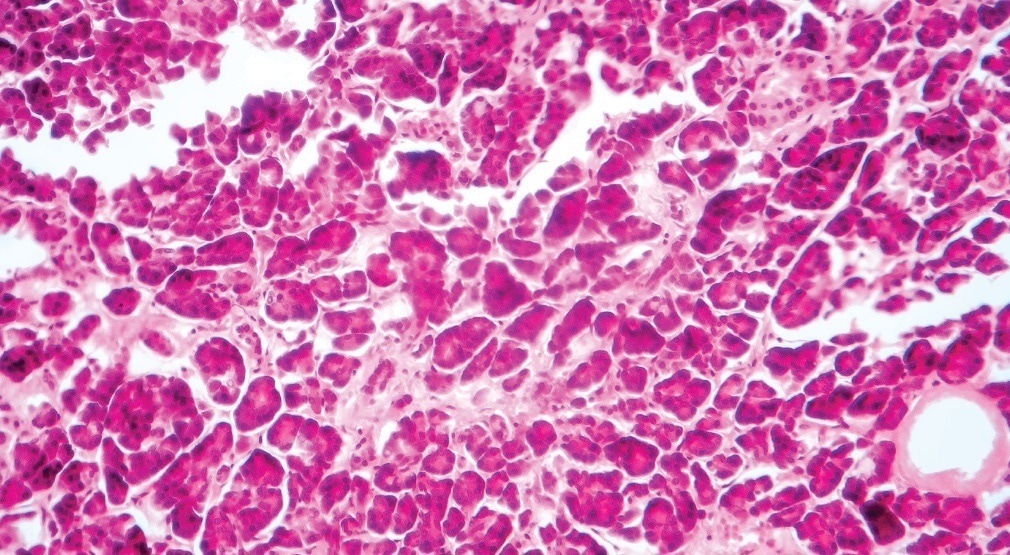
Image Credit: Van Andel Institute
ß cells play an important role in maintaining the body's metabolic equilibrium. They are the only cells that can produce insulin, which controls blood sugar levels by assigning dietary sugar for immediate or long-term usage.
In Type 1 diabetes, the body’s own immune system attacks ß cells, making them unable to generate insulin.
Insulin resistance causes type 2 diabetes; increased blood sugar from a person’s diet pushes ß cells in the pancreas to work overtime. When ß cells can no longer keep up, blood sugar levels could reach dangerously high levels.
Both diseases are treated by increasing insulin activity, either by delivering more insulin or by increasing its activity and release into the bloodstream. Some people with Type 1 diabetes may choose to have a ß cell transplant, which is an experimental operation in which functioning cells from a donor are inserted into the pancreas.
The new results, published in Cell Metabolism, point to a number of potential directions for future diabetes therapies, such as changing the ratio of ß cell subtypes in transplants to guarantee optimal performance.
All cells vary in some way, but these two ß cell subtypes are discretely and consistently different from one another. This indicates that they serve two different but necessary functions as insulin producers. They are specialists, each with their own roles.”
Dr J. Andrew Pospisilik, Study Senior Author and Professor, Van Andel Institute
He added, “We also see differences in the ratio of one subtype to another in diabetes. Understanding these two cell types—and their relationship to each other—gives us a clearer picture of diabetes and offers new opportunities for treatment.”
Scientists have always recognized variances amongst ß cells, but this is the first research to identify particular cell subtypes. The findings were discovered in mice models and also in human ß cell samples.
The two types, known as ßHI and ßLO, differ in a particular function, size, shape, and epigenomic traits, among other things. They also have different patterns of surface markers, which let cells transmit and receive chemical information. Type 2 diabetes appears to have a higher prevalence of ßHI cells.
Importantly, the presence or lack of a protein called CD24, which works as a marker that permits targeting of one type but not the other, can distinguish the subtypes. This differentiation could help in the creation of more accurate diabetes treatment techniques and provides a key tool for diabetes researchers to thoroughly analyze each cell type.
The discoveries change the understanding of how ß cells form early in life. With lifespans of 30 to 40 years, ß cells are among the most durable cells in the body.
The earliest ß cells develop from stem cells, which are blank cells that differentiate into the many cell types that comprise the body, just like all other cells. Transcription factors are specialized proteins that control the “on” and “off” switching of genes, and they play a major part in this process.
The study proposes that ß cells could be an exception. The choice of ß cells to become ßHI or ßLO was determined by epigenetic dosage rather than transcription factors, according to the research. The dose of epigenetic factors has never before been demonstrated to alter the proportion of related cell types.
Epigenetic markers, like transcription factors, instruct genes when to be active and when to be inactive. The number of these markers is referred to as the epigenetic dose. The group earlier discovered an epigenetic mark termed H3K27me3 as an important driver of differentiation in ß cells.
In this recent study, researchers discovered that the dose of the same mark regulates ßHI vs ßLO numbers, providing a new target for potentially effective diabetes therapies.
Pospisilik concluded, “The beauty of this mechanism is its novelty—it is purely driven by epigenetics with no help from transcription factors. The key here is that epigenetic changes can be reversed, which opens a whole host of questions with implications for treatment.”
Source:
Journal reference:
Dror, E., et al. (2023). Epigenetic dosage identifies two major and functionally distinct β cell subtypes. Cell Metabolism. doi.org/10.1016/j.cmet.2023.03.008