 By Pooja Toshniwal PahariaReviewed by Lexie CornerMay 30 2025
By Pooja Toshniwal PahariaReviewed by Lexie CornerMay 30 2025A recent study published in Cancer Gene Therapy examined the genetic contributions of mesenchyme homeobox 2 (MEOX2) and switch/sucrose non-fermentable-related matrix-associated actin-dependent regulator of chromatin subunit B1 (SMARCB1) in lung cancer.
The results suggest that MEOX2 is associated with tumor growth promotion, while SMARCB1 appears to act as a tumor suppressor. These genes may have relevance in assessing prognosis and guiding treatment approaches in lung cancer.
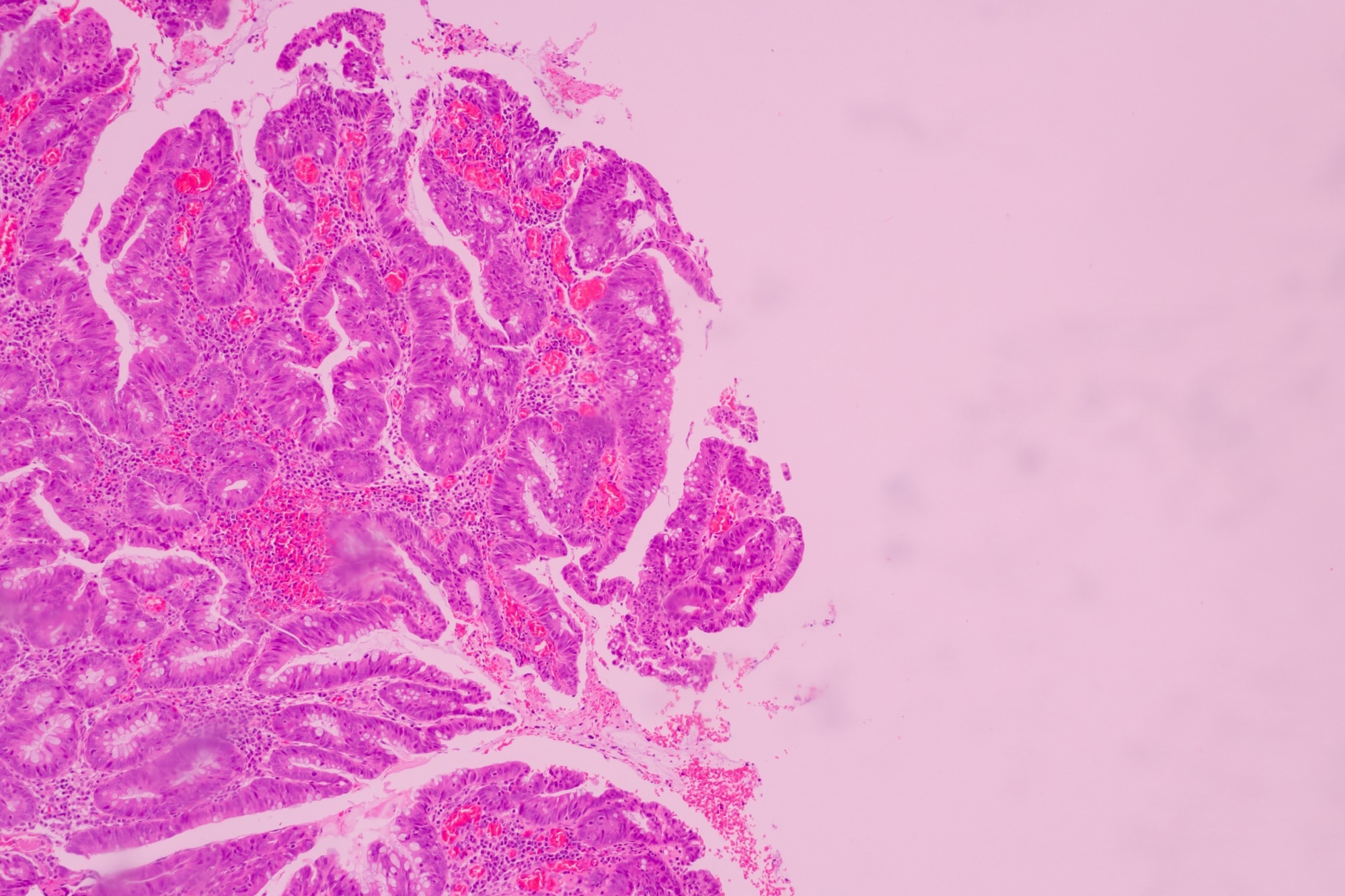
Image Credit: Komsan Loonprom/Shutterstock.com
Background
Lung cancer remains one of the leading causes of cancer-related mortality globally. Previous studies have identified GLI family zinc finger-1 (GLI-1), SMARCB1, and MEOX2 as potentially important in lung cancer development, but the specific molecular roles of these genes are not fully understood.
MEOX2 encodes transcription factors involved in homeobox activity, which contributes to developmental processes and tissue repair. It has also been linked to tumor-related processes, including proliferation, invasion, angiogenesis, metastasis, and treatment resistance. MEOX2 influences GLI-1 expression through Sonic Hedgehog (Shh) signaling, a pathway implicated in cell growth regulation.
Both MEOX2 and SMARCB1 are thought to influence epidermal growth factor receptor (EGFR) expression, which plays a role in non-small cell lung carcinoma (NSCLC) progression.
Study Design and Methods
This study investigated the roles of SMARCB1, GLI-1, and MEOX2 genes in lung cancer pathogenesis, focusing on their influence on epigenetic modifications of oncogenes such as EGFR and the resulting impact on the effectiveness of tyrosine kinase inhibitor (TKI) therapies.
The researchers conducted short hairpin RNA (shRNA)–mediated gene silencing of GLI-1, SMARCB1, and MEOX2 in two human lung cancer cell lines: A549 (lung adenocarcinoma) and NCI-H1975 (non-small cell lung cancer, NSCLC). RNA and protein were extracted from the cells for downstream analysis.
Messenger RNA (mRNA) expression levels were quantified using quantitative polymerase chain reaction (qPCR), while Western blotting and chemiluminescence were used to assess EGFR protein expression.
Cells were treated with afatinib, an EGFR-targeted TKI, to evaluate the effects of gene silencing on drug sensitivity. Cell viability was measured using the MTT assay.
For in vivo experiments, 5.0 × 10⁶ shRNA-transduced A549 cells in 0.1 mL were subcutaneously injected into mice. Tumor growth was monitored before and after daily administration of TKIs (erlotinib or afatinib) at a dose of 10 mg/kg for seven days. Assessments included measurements of tumor volume, body weight, and signs of physical distress (e.g., vomiting, skin ulceration, and impaired mobility).
Chromatin immunoprecipitation (ChIP) assays were performed using pulverized tumor tissue to evaluate chromatin changes associated with EGFR and GLI-1 expression. These assays aimed to elucidate regulatory mechanisms involving SMARCB1.
To relate the experimental data to clinical observations, the team analyzed The Cancer Genome Atlas (TCGA) data from early-stage lung cancer cases. Progression-free interval (PFI) curves were generated for patients receiving TKI treatment. Additionally, protein–protein interaction analyses were conducted using the STRING database to explore molecular interactions involving the studied genes.
Results
Gene silencing of GLI-1 and MEOX2 reduced H3K27Ac levels—a marker of active chromatin—at the EGFR gene locus in NSCLC cells. This suggests that MEOX2 may contribute to lung cancer progression through epigenetic modulation involving CREB-binding protein (CBP).
MEOX2 silencing also appeared to enhance sensitivity to TKI treatment. TCGA data supported these findings by showing improved survival in patients with low MEOX2 expression who received EGFR-targeted therapy.
SMARCB1, on the other hand, was found to inhibit tumor growth and improve responsiveness to TKIs. Silencing SMARCB1 increased EGFR expression via reduced H3K27me3 (a repressive epigenetic mark) and elevated EZH2 levels. This state of reduced repression also led to activation of oncogenes via BRD9, part of the non-canonical BAF (ncBAF) complex. Inhibiting BRD9 may enhance treatment response in SMARCB1-deficient tumors.
SMARCB1 deficiency was associated with reduced efficacy of afatinib treatment. Patients with higher SMARCB1 levels showed improved progression-free intervals (62 months vs. 27 months). MEOX2 silencing appeared to increase SMARCB1 expression at enhancer regions near the EGFR locus, suggesting a regulatory relationship.
Download your PDF copy now!
Conclusion
The study identifies opposing roles for SMARCB1 and MEOX2 in lung cancer: SMARCB1 acts as a tumor suppressor and enhances therapeutic response, while MEOX2 promotes tumor progression and is associated with reduced drug sensitivity. These genes may serve as biomarkers for predicting response to EGFR-targeted therapies and as potential targets for future therapeutic strategies.
Journal Reference
Trejo-Villegas, O.A., et al. (2025). SMARCB1-driven EGFR-GLI1 epigenetic alterations in lung cancer progression and therapy are differentially modulated by MEOX2 and GLI-1. Cancer Gene Ther. DOI: 10.1038/s41417-025-00873-0, https://www.nature.com/articles/s41417-025-00873-0