 By Pooja Toshniwal PahariaReviewed by Lexie CornerJun 2 2025
By Pooja Toshniwal PahariaReviewed by Lexie CornerJun 2 2025A study published in Advanced Healthcare Materials describes the bioengineering of three-dimensional (3D) kidney glomerular microtissues that replicate the glomerular filtration barrier (GFB) structure and mechanical environment.
The model was developed to support studies of podocyte-related diseases by simulating biomechanical forces important to podocyte health. This system offers a platform for studying podocyte behavior and assessing potential drug targets for podocytopathies more realistically than conventional two-dimensional cultures.
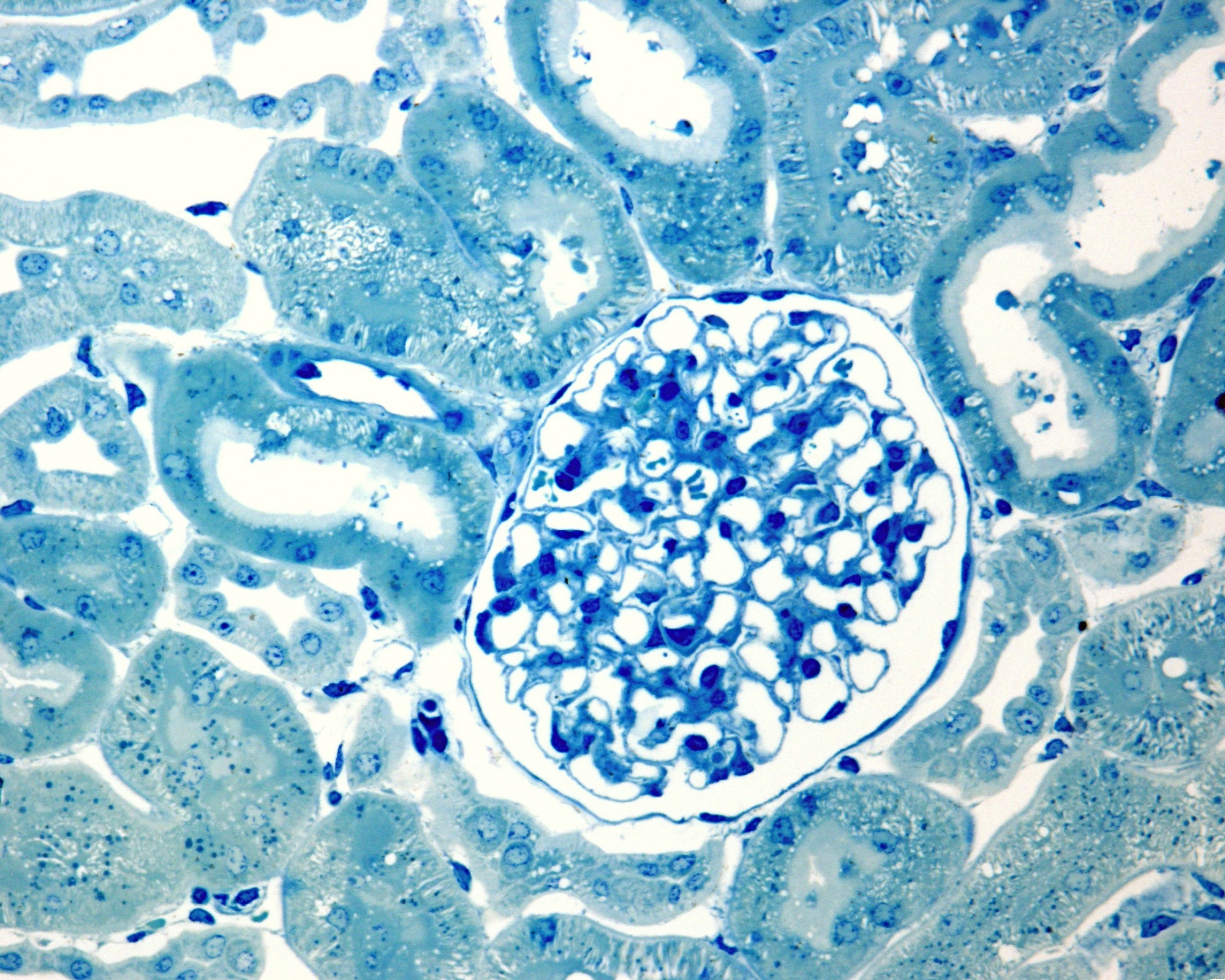 Image Credit: Jose Luis Calvo/Shutterstock.com
Image Credit: Jose Luis Calvo/Shutterstock.com
Background
Podocytes are specialized epithelial cells in the kidney glomerulus that contribute to the function and integrity of the GFB. They help filter waste products while preventing the loss of large molecules such as proteins in urine.
Podocytes experience mechanical forces that influence their structural adaptation. In response, they remodel their cytoskeleton to maintain adhesion with the extracellular matrix (ECM). A failure to adapt to these mechanical forces can result in podocytopathies, which are associated with proteinuria and impaired kidney function.
There remains a need for in vitro models that accurately replicate human GFB architecture and mechanobiology. Existing models often lack a mature glomerular basement membrane (GBM) and do not simulate the mechanical forces present in the kidney.
About the Study
The researchers developed a 3D microtissue model of the human glomerulus to investigate podocyte injuries under controlled laboratory conditions.
They evaluated podocyte mechanical resilience in response to both chemical and genetic stressors. Podocyte injury was modeled using a doxycycline-inducible transient receptor potential canonical 6 (TRPC6) mutation, known to cause calcium overload. The potential therapeutic effects of SAR7334, a TRPC6 inhibitor, were also assessed.
The 3D structure was constructed using polydimethylsiloxane (PDMS) microwells (3.6 mm × 1.8 mm × 2.0 mm) containing two vertically aligned flexible micropillars (500 μm diameter, 1.8 mm apart). Human endothelial cells were mixed with ECM components, including type I collagen, and cultured in these wells. Within 24 hours, podocytes began spreading and compacting the ECM. Deflection of the micropillars indicated contractile force generation and cytoskeletal remodeling.
The model was subjected to low (2.5 %) and high (12 %) strain conditions to mimic physiological and pathological mechanical forces, respectively.
Human conditionally immortalized podocytes (ciPods) were used to generate compressive forces on endothelial microtissues. Treatments with vascular endothelial growth factor A (VEGF-A) and thrombin were applied to evaluate changes in biomechanical stress distribution. Tissue organization was assessed using immunofluorescence, confocal, and two-photon microscopy. Gene expression changes were measured after treatment with tumor necrosis factor-alpha (200 ng/ml for seven days), a cytokine associated with podocyte injury.
Results
The engineered model replicated the three-layered glomerular architecture, including endothelial cells, basement membrane, and overlying podocytes. Podocytes adhered to the GBM through interdigitated foot processes and actin filaments, applying significant compressive forces (26 %) to the endothelial layer. However, slit diaphragms—key filtration structures—were not observed in the current model.
Under low strain (2.5 %, 20 kPa), podocytes maintained adhesion to the GBM and exerted tensile forces via integrin-mediated interactions with ECM proteins such as laminin and collagen IV. High strain conditions (12 %, 128 kPa) mimicking hypertension and hyperfiltration resulted in podocyte detachment and reduced force generation.
Compared to thrombin and VEGF-A, podocytes exerted stronger compressive forces and upregulated expression of podocyte markers such as synaptopodin (SYNPD) and podocalyxin-like (PODXL). In contrast, TNFα treatment reduced contractile force, induced cell elongation, and increased expression of pro-apoptotic genes, including RARRES1, which are associated with podocyte dysfunction.
TRPC6 activation decreased podocyte contractile forces by approximately 30 % over eight days, disrupting actin stability. Treatment with 10 μM SAR7334 for two days partially restored contractility, suggesting TRPC6 inhibition may be a potential therapeutic strategy. These results support the model’s utility for studying podocyte behavior and screening drug candidates.
Download your PDF copy now!
Conclusion
The study presents a 3D microtissue model that recapitulates key aspects of the glomerular structure and podocyte mechanics. The model enables analysis of podocyte responses to mechanical and biochemical stress and may serve as a tool for validating therapeutic targets in podocytopathies.
Future work should aim to incorporate patient-derived cells, apply perfusion and shear stress, and develop podocytes that form slit diaphragms to enhance physiological relevance. These developments may improve the model’s utility for studying kidney diseases and advancing personalized therapeutic approaches.
Journal Reference
Buttό, S. (2025). Engineered 3D Kidney Glomerular Microtissues to Model Podocyte-Centric Diseases for the Validation of New Drug Targets. Adv. Healthcare Mater. DOI: 10.1002/adhm.202404767, https://advanced.onlinelibrary.wiley.com/doi/10.1002/adhm.202404767