Reviewed by Lexie CornerJun 23 2025
Scientists have long known that the Alzheimer’s brain contains abnormal plaques and tangles. Recent research has also highlighted the role of the brain’s vascular system in the progression of the disease.
However, for decades, these findings have not led to fully effective treatments. Despite important discoveries, the exact process of neurodegeneration is still not fully understood.
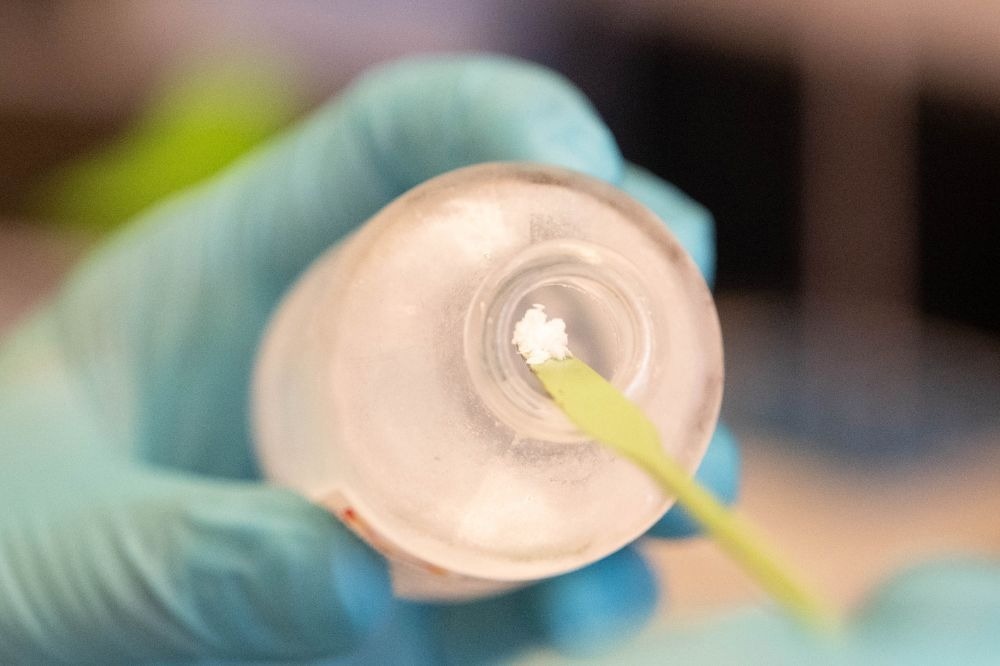 The study used purified human fibrinogen, pictured here. Image Credit: Lori Chertoff/The Rockefeller University
The study used purified human fibrinogen, pictured here. Image Credit: Lori Chertoff/The Rockefeller University
New research shows that Aβ binds to fibrinogen, a key blood protein. This interaction creates abnormal clots that are difficult to break down. These clots are linked to vascular damage and inflammation. Even small amounts of this complex appear to trigger early signs of Alzheimer’s, including synapse loss, neuroinflammation, and disruption of the blood-brain barrier.
The study reinforces the link between vascular disease and neurodegeneration. It also points to a possible treatment target for Alzheimer’s: the Aβ/fibrinogen complex.
It takes a larger amount of Aβ or fibrinogen alone to cause serious damage in the Alzheimer’s brain. But when the two complex together, you only need very small amounts of each to cause damage. There is a synergistic effect with Aβ and fibrinogen.
Erin Norris, Research Associate Professor, Rockefeller University
Compounding the Problems
Strickland's Patricia and John Rosenwald Laboratory of Neurobiology and Genetics has been studying the Aβ/fibrinogen complex for nearly 20 years. Earlier studies showed that Aβ attaches to fibrinogen and contributes to Alzheimer’s development. Their work revealed a connection between neurodegeneration and vascular health. This idea was once debated but has gained broader acceptance since the team first proposed it.
Norris added, “Only recently, with a number of breakthroughs in the field, did people begin to believe that the vascular system is involved in AD pathogenesis. Since our initial findings, we have been focused on studying the mechanisms that explain how a dysfunctional vascular system impacts AD.”
Identifying the Aβ/fibrinogen complex was a valuable first step. However, the extent of its effects - and whether the complex alone can cause Alzheimer’s - remains unclear. To investigate further, Strickland’s team created the compound in the lab at low concentrations. They then applied it directly to mouse brain tissue slices and live brain cells. The goal was to closely study the impact of Aβ/fibrinogen.
We wanted to really show the damage, to zoom in on exactly how pre- and post-synaptic terminals were being harmed.
Elisa Nicoloso Simões-Pires, Research Associate, Rockefeller University
They found that the combination of low levels of Aβ and fibrinogen was harmful to synapses. It also triggered several key features of Alzheimer’s disease, including neuroinflammation and blood-brain barrier disruption. In contrast, either Aβ or fibrinogen alone, even at higher doses, caused little damage.
The researchers then used antibodies to block Aβ from binding to fibrinogen. This reduced the harmful effects, confirming that the Aβ/fibrinogen complex was responsible.
“We showed that the complex actually induces blood-brain barrier leakage, when the proteins alone did not. Disruption of the blood-brain barrier allows for blood proteins to cross into the brain, which leads to additional harm,” Simões-Pires added.
A New Drug Target
One strength of the study was its use of both live mice and brain slices.
“It was an in vitro and in vivo project, both providing the same outcome. We are much more confident in our results when we can show the same thing in culture and a living organism,” Norris noted.
The group now plans to investigate the mechanism behind the findings. They aim to understand why this complex causes such harmful effects.
The study suggests that even small amounts of the Aβ/fibrinogen combination can produce Alzheimer’s-like features well before cognitive symptoms appear. This could have clinical implications. For instance, phospho-tau181 - a biomarker used to detect Alzheimer’s years before symptoms arise in humans - was also elevated in mice exposed to the compound.
This result indicates that the study may be modeling the early stages of Alzheimer’s disease. It also suggests that early intervention targeting the complex could potentially delay or prevent disease development.
Although many factors contribute to Alzheimer’s, the team believes this specific pathway deserves further investigation.
Simões-Pires emphasized, “It is not a simple disease. A lot of other factors can induce neurotoxicity, and we certainly do not propose that inhibiting this complex formation would cure AD. But perhaps targeting this complex would alleviate some of the pathologies and be even more effective in combination with other therapies.”
Source:
Journal reference:
Kang, J. S., et al. (2025) Exercise-induced CLCF1 attenuates age-related muscle and bone decline in mice. Nature Communications. doi.org/10.1038/s41467-025-59959-w.