 By Pooja Toshniwal PahariaReviewed by Lauren HardakerAug 6 2025
By Pooja Toshniwal PahariaReviewed by Lauren HardakerAug 6 2025In a recent study published in Frontiers in Immunology, researchers developed a fragment crystallizable (Fc)-optimized monoclonal antibody (mAb), 8H8_SDIE, targeting the cluster of differentiation 276 (CD276) antigen of non-small cell lung cancers (NSCLC). The mAb activates natural killer (NK) cells to lyse tumor cells through enhanced antibody-dependent cellular cytotoxicity (ADCC). The findings suggest 8H8_SDIE as a potential therapeutic option for patients with CD276-positive NSCLC tumors recalcitrant to conventional T cell-stimulating immune checkpoint inhibitors (ICIs).
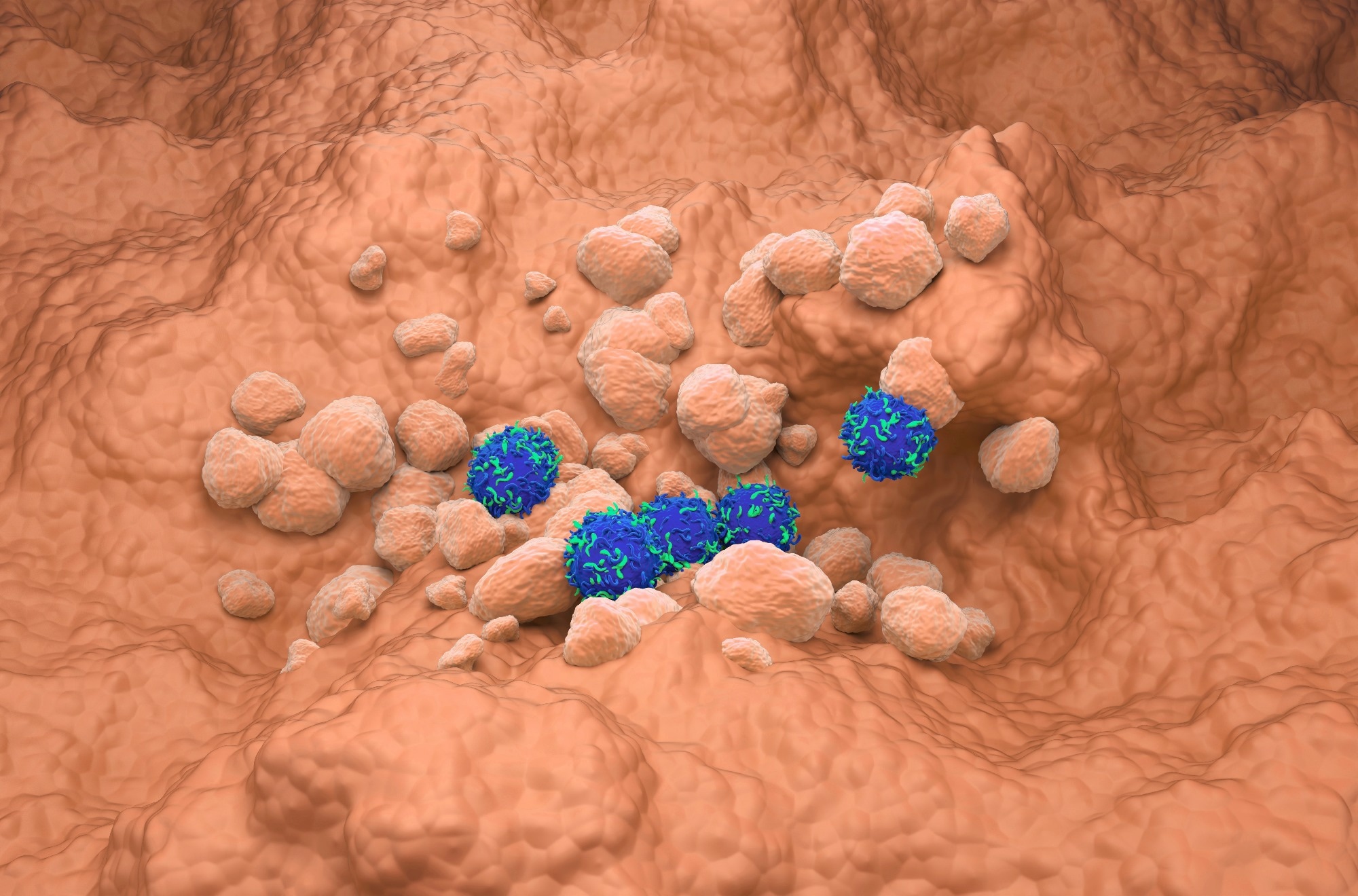 Study: Fc-optimized CD276 antibody enhances NK cell activation against non-small cell lung cancer. Image credit: Nemes Laszlo/Shutterstock.com
Study: Fc-optimized CD276 antibody enhances NK cell activation against non-small cell lung cancer. Image credit: Nemes Laszlo/Shutterstock.com
NSCLC is a common and fatal cancer globally, with poor prognostic rates for patients with late-stage tumors. ICIs have revolutionized NSCLC treatment; however, a few subgroups develop resistance, limiting therapeutic benefits. Despite a lower toxicity rate than conventional chemotherapeutic agents, many patients suffer severe autoimmune adverse effects from broad immunological stimulation that can affect multiple organs. There is an unmet need for innovative strategies for patients unresponsive to standard immunotherapeutic regimens.
ICIs targeting programmed cell death protein 1 (PD-1) and its ligand (PD-L1) improve treatment outcomes but are less effective in certain tumors. Studies report CD276 expression in NSCLC tumors that lack PD-L1, which is particularly relevant for patients who do not benefit from PD-1/PD-L1 inhibitors. Importantly, CD276 exhibits tumor-specific expression in NSCLC and low expression in normal tissues, which makes it a promising candidate for NSCLC immunotherapy.
About the Study
In the present study, researchers analyzed CD276 antigen expression by NSCLC cells. They investigated the efficacy of 8H8_SDIE, an Fc-engineered anti-CD276 antibody, in expanding the therapeutic landscape of NSCLC by enhancing the actions of NK cells.
The team isolated peripheral blood mononuclear cells (PBMCs) from healthy donors through centrifugation and maintained them in RPMI culture medium under controlled conditions of 37°C and 5.0% CO₂. They obtained A549, NCI-H226, and NCI-H460 cells to represent NSCLC, verified for authenticity by immunophenotyping.
The researchers assessed CD276 messenger ribonucleic acid (mRNA) expression in NSCLC cells using The Cancer Genome Atlas (TCGA) datasets, including lung adenocarcinoma (54 regular tissue and 491 primary tumor) and squamous cell carcinoma (51 normal tissue and 501 tumor) samples. Using TCGA data, they determined the influence of CD276 levels on patients' overall survival (OS) rates. High CD276 expression was associated with significantly shorter OS in adenocarcinoma; in squamous cell carcinoma, the trend was similar but did not reach statistical significance.
The team generated 8H8_SDIE with an optimized Fc region by incorporating S239D/I332E mutations. Protein affinity and preparative size exclusion chromatography refined the antibody, and analytical size exclusion chromatography confirmed purity and quality.
CD3 and CD56 antigens identified NK cells, CD69-PE and CD25-PE levels indicated their activation, and CD107a expression indicated degranulation. Flow cytometry revealed the expression of cytokines, such as tumor necrosis factor (TNF), interleukin-2 (IL-2), and IL-10. The assays also demonstrated the secretion of cytotoxic granzymes, perforin, and granulysin in NK cells stained with fluorescence-labeled antibodies, CD3-APC and CD56-PE/Cy7. Enzyme-linked immunosorbent assays (ELISA) revealed interferon-gamma (IFN-γ) expression.
PBMCs cultured with the NSCLC cell lines in a 2.5:1 effector-to-target (E:T) ratio for activation assays using 200,000 NSCLC cells and 500,000 PBMCs treated with 1.0 µg/mL antibody, demonstrated NK cell activity. NK cell cytotoxicity was measured at 15-minute intervals over 150 hours, in a separate long-term assay using NSCLC cell-PBMC co-culture at a 40:1 E:T ratio, with or without the mAb.
Results
Flow cytometry showed low, moderate, and high CD276 expression in NCI-H460, NCIH-226, and A549 cells. Elevated CD276 expression was associated with a shorter OS (median) of 39 months and a two-fold increase in mortality risk among lung adenocarcinoma patients. For squamous cell carcinoma, high CD276 expression showed a similar but non-significant trend towards poorer OS. The findings confirm the prognostic role of CD276 in lung malignancies.
The team found that 8H8_SDIE specifically binds to CD276 antigens on NSCLC cells, significantly activating NK cells, demonstrating increased degranulation. They released antitumoral cytokines such as IFN-γ and TNF and cytotoxic molecules like granzyme B and perforin. Fc receptor optimization improved ADCC by enhancing CD16a binding on NK cells while reducing inhibitory FcgRIIb receptor interactions. Real-time imaging over 150 hours confirmed robust and sustained target cell lysis mediated by 8H8_SDIE.
Unlike conventional CD276-targeting ADCs, 8H8_SDIE induces potent NK cell-mediated cytotoxicity exclusively through immune effector engagement, without cytotoxic payloads, potentially reducing systemic toxicity and off-target effects. While the study suggests that this approach could preserve anti-tumor effects without ADC-related toxicities, direct head-to-head efficacy comparisons with ADCs in NSCLC models were not performed.
The payload-free design avoids the dose-limiting toxicities associated with ADCs, offering a safer and more clinically viable approach. In AML in vivo models from prior work, no signs of off-target immune activation or cytokine release were observed; however, such safety data are not yet available for NSCLC.
Conclusions
Based on the findings, 8H8_SDIE represents an appealing next-generation strategy for treating CD276-positive, ICI-resistant NSCLC. This approach can strengthen NK cell activity while minimizing toxicity and resistance associated with current checkpoint inhibitors, offering hope for patients who do not respond to anti-PD-1 or anti-PD-L1 treatments.
The authors emphasize that translating these findings into clinical success will require advanced in vivo NSCLC models to confirm safety and efficacy and optimize NK cell persistence and delivery. Future studies could evaluate combinatorial approaches with ICIs and biodistribution profiles to determine the long-term efficacy and safety of NK cell therapies such as 8H8_SDIE.
Download your PDF copy now!
Journal Reference
Stefan´czyk SA et al. (2025). Fc-optimized CD276 antibody enhances NK cell activation against non-small cell lung cancer. Front. Immunol., 16:1624751. DOI: 10.3389/fimmu.2025.1624751 https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1624751/full