 By Pooja Toshniwal PahariaReviewed by Lauren HardakerOct 29 2025
By Pooja Toshniwal PahariaReviewed by Lauren HardakerOct 29 2025In a new clinical trial, scientists used a wireless photovoltaic implant to restore meaningful central vision in patients once thought permanently blind from macular degeneration. 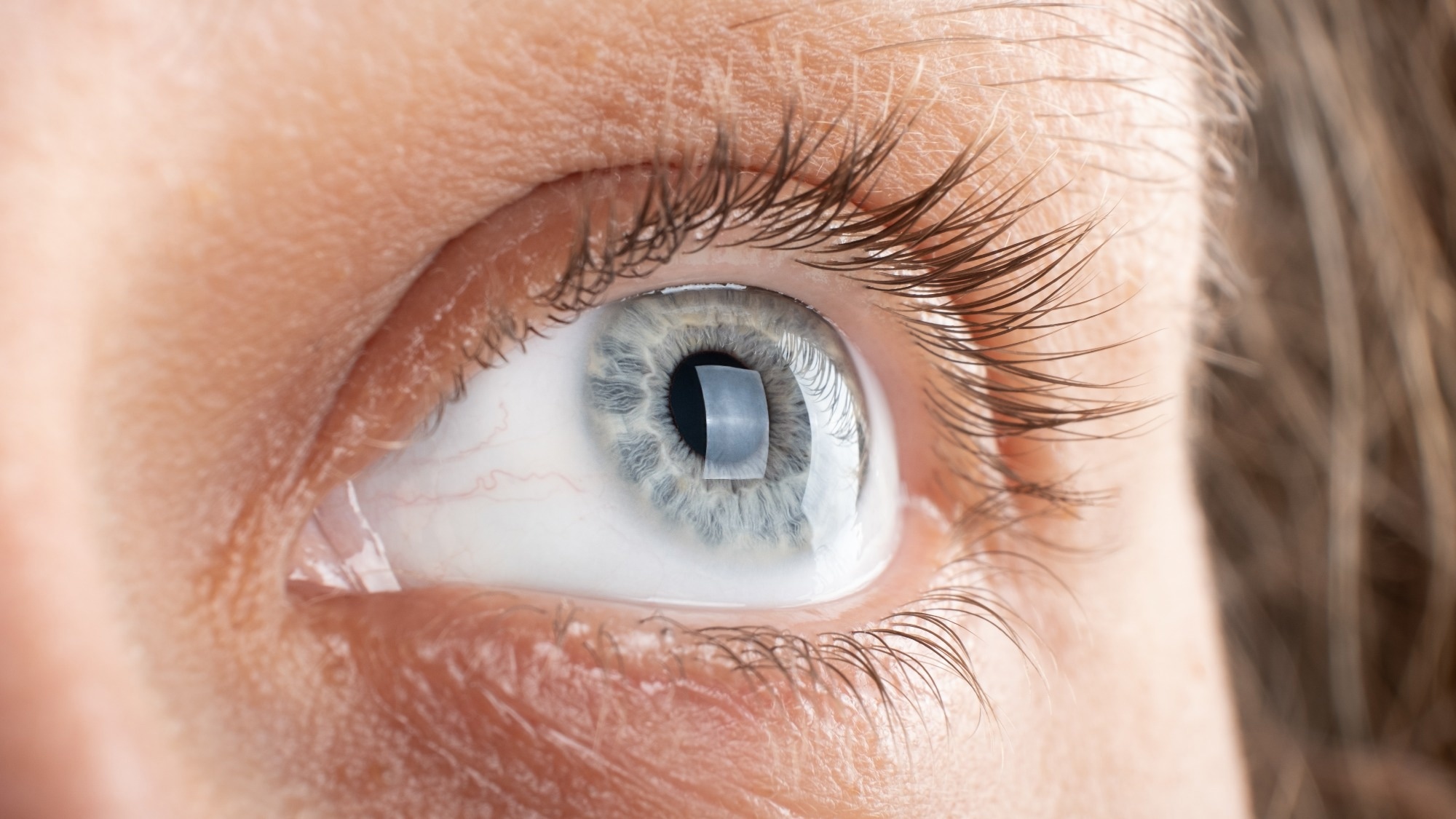
Image credit: fukume/Shutterstock.com
A recent study published in The New England Journal of Medicine reports that the subretinal photovoltaic retina implant microarray (PRIMA) system can partially restore central vision function in patients with advanced age-associated macular degeneration (AMD).
Over 12 months, 81% of participants suffering from geographic atrophy (GA) showed significant gains in visual acuity, with some regaining the ability to read letters and words at home. By wirelessly restoring photoreceptor function while preserving residual peripheral vision, the PRIMA implant system represents a significant advance toward reversing aspects of previously irreversible central blindness.
AMD is a major driver of permanent blindness in aging populations. Its advanced form, GA, causes loss of photoreceptors and retinal pigment epithelium. While new complement inhibitors such as pegcetacoplan and avacincaptad pegol can slow disease progression, none can restore lost vision.
The PRIMA approach introduces a novel approach to restoring photoreceptor function through targeted neurostimulation. It uses an untethered subretinal implant paired with specialized glasses. The implant converts projected light from the near-infrared (NIR) spectrum into electrical signals that activate retinal neurons, reestablishing visual transmission to the brain while maintaining residual peripheral vision.
About the Study
In this open-label, multicenter clinical trial (PRIMAvera study), researchers evaluated the safety and efficacy of the PRIMA implant system in restoring central vision among patients with GA secondary to AMD. The trial was conducted across 17 sites in five European nations and built upon earlier feasibility data demonstrating measurable visual improvement with PRIMA implants.
Eligible participants were aged ≥60 years, had bilateral GA verified by optical coherence tomography (OCT) and autofluorescence imaging, and presented with visual clarity (acuity) of ≥1.2 logMAR (20/320 Snellen). The atrophic area in the eye exceeded a diameter of 2.40 mm, ensuring complete coverage of the implant within the lesion.
The researchers surgically placed the PRIMA implant within the atrophic region of the study eye. Following implantation, participants underwent visual assessments at six months and one year, both with PRIMA glasses and without. During testing, participants could freely adjust zoom and brightness settings.
The primary endpoint was a meaningful enhancement in visual clarity, defined as a gain of ≥0.20 logMAR (10 or more letters) on the Early Treatment Diabetic Retinopathy Study (ETDRS) chart after one year. Secondary endpoints included visual clarity at six months, changes in mean visual acuity over time, patient-reported outcomes, assessed using the Impact of Vision Impairment (IVI) survey, and evaluation of central vision improvement after 12 months.
Safety outcomes included the frequency and extent of device- or procedure-related serious-type adverse events within 12 months. Post-surgical assessments included implant-resolution testing using Landolt C optotypes to measure device resolution independently of digital processing.
At 12 months, participants completed a 19-item survey on home use, capturing the system’s practicality and impact on everyday visual tasks. Of 38 PRIMA implant recipients, 32 (mean age, 79 years) completed the evaluation; the remaining withdrew, died, or were unavailable.
Results
Within a year, 26 participants (81%) achieved a clinically significant enhancement in visual clarity, defined as a gain of at least 0.2 logMAR (≥10 letters) from baseline. After accounting for missing data, the overall estimated improvement rate was 80%.
The mean gains in visual clarity were 0.49 logMAR and 0.51 logMAR with PRIMA glasses and the participant’s preferred condition, corresponding to mean improvements of 25 and 26 letters, respectively. The maximum improvement observed was 1.18 logMAR (59 letters). At six months, 57% of participants showed comparable improvements, confirming sustained visual benefit.
After one year, nearly all participants (94%) demonstrated central visual perception with the PRIMA system. Post-surgical evaluation yielded a mean acuity of 1.32 logMAR (20/417 Snellen), consistent with the implant’s theoretical optical limit.
In addition, 84% successfully used prosthetic vision at home for reading letters, numbers, and words, and 69% reported moderate to high satisfaction with the system. However, results from the IVI questionnaire did not indicate measurable behavioral or quality-of-life changes, and the study was not powered to detect such differences. Digital enhancements, such as contrast, brightness, and zoom adjustments, improved object recognition across varying lighting conditions.
The team noted 26 serious-type adverse events in 19 individuals related to surgical and implantation procedures; none were from device use. Most (81%) were reported within two months post-surgery and resolved quickly. Common events included ocular hypertension (23%), retinal breaks, macular holes, and subretinal hemorrhage, all successfully managed. Two choroidal neovascularization cases were treated effectively with vascular endothelial growth factor (VEGF)-targeting injections. Most adverse events (85%) were mild or moderate in severity, and none were life-threatening.
Based on the findings, the PRIMA implant can safely and effectively restore meaningful improvements in central vision acuity in patients with AMD-related GA, once considered untreatable. By reactivating the blind central retina while preserving peripheral vision, the system enables tasks such as reading and letter recognition, enhancing patient independence and quality of life. Although further research is needed to confirm long-term efficacy and functional benefits, the system's wireless, upgradeable design means PRIMA offers a scalable platform for next-generation vision restoration, marking a remarkable step forward in treating degenerative retinal diseases.
Journal Reference
F.G. Holz et al. (2025). Subretinal Photovoltaic Implant to Restore Vision in Geographic Atrophy Due to AMD, N Engl J Med, DOI: 10.1056/NEJMoa2501396. https://www.nejm.org/doi/10.1056/NEJMoa2501396