Reviewed by Lauren HardakerJan 28 2026
Gene-editing techniques such as CRISPR have enabled new treatments for previously incurable diseases. Researchers at the University of British Columbia are now expanding those capabilities to include the skin for the first time.
 Study: Corona Borealis Studio
Study: Corona Borealis Studio
The UBC team, working with researchers from the Berlin Institute of Health at Charité in Germany, created the first gene therapy capable of repairing defective genes when administered directly to human skin.
The result, described in a report published in Cell Stem Cell, might lead to new treatments for a wide range of hereditary skin conditions, including uncommon inherited diseases and more prevalent disorders such as eczema.
With this work, we show that it is possible to correct disease-causing mutations in human skin using a topical treatment that is safe, scalable and easy-to-use. Importantly, the approach corrects the root cause of disease, and our data suggests that a one-time treatment might even be enough to provide a lasting and durable cure.
Dr. Sarah Hedtrich, Study Senior Author and Associate Professor, School of Biomedical Engineering, University of British Columbia
Broad Therapeutic Potential
The study demonstrates that gene therapy can cure the most frequent genetic mutation causing autosomal recessive congenital ichthyosis (ARCI), a rare and life-threatening hereditary skin condition that emerges at birth.
ARCI affects around one in every 100,000 people and produces permanent consequences such as severely dry and scaly skin, persistent inflammation, and an increased risk of infection. There is presently no cure or effective therapy; sufferers must deal with their symptoms for the rest of their lives.
For many patients, this condition is not only physically painful, but also deeply stigmatizing and isolating.
Dr. Sarah Hedtrich, Study Senior Author and Associate Professor, School of Biomedical Engineering, University of British Columbia
By testing the treatment on models of actual human skin, the researchers demonstrated that it can restore up to 30 % of normal skin function, a number that prior research shows might be clinically important for restoring skin function to normal.
While ARCI affects a small number of people, the researchers believe the treatment strategy could be applied to a variety of other genetic skin diseases, including epidermolysis bullosa, a severe skin blistering condition also known as ‘butterfly skin’, and potentially more common conditions like eczema or psoriasis.
“The approach we developed is a platform technology. It can be readily adapted to treat almost any skin disease,” added Dr. Hedtrich.
 Dr. Sarah Hedtrich (center) and her team examine a skin-on-a-chip model used to test the new CRISPR-based therapy on living human skin samples. Image Credit: UBC Faculty of Medicine
Dr. Sarah Hedtrich (center) and her team examine a skin-on-a-chip model used to test the new CRISPR-based therapy on living human skin samples. Image Credit: UBC Faculty of Medicine
A New Way to Deliver CRISPR Gene Editing
Despite significant improvements in gene editing, applying the technique to skin diseases has long been a barrier. The skin's fundamental function is to shield the body from the outside environment, making it difficult to transfer big biological remedies like gene editing across its protective barrier.
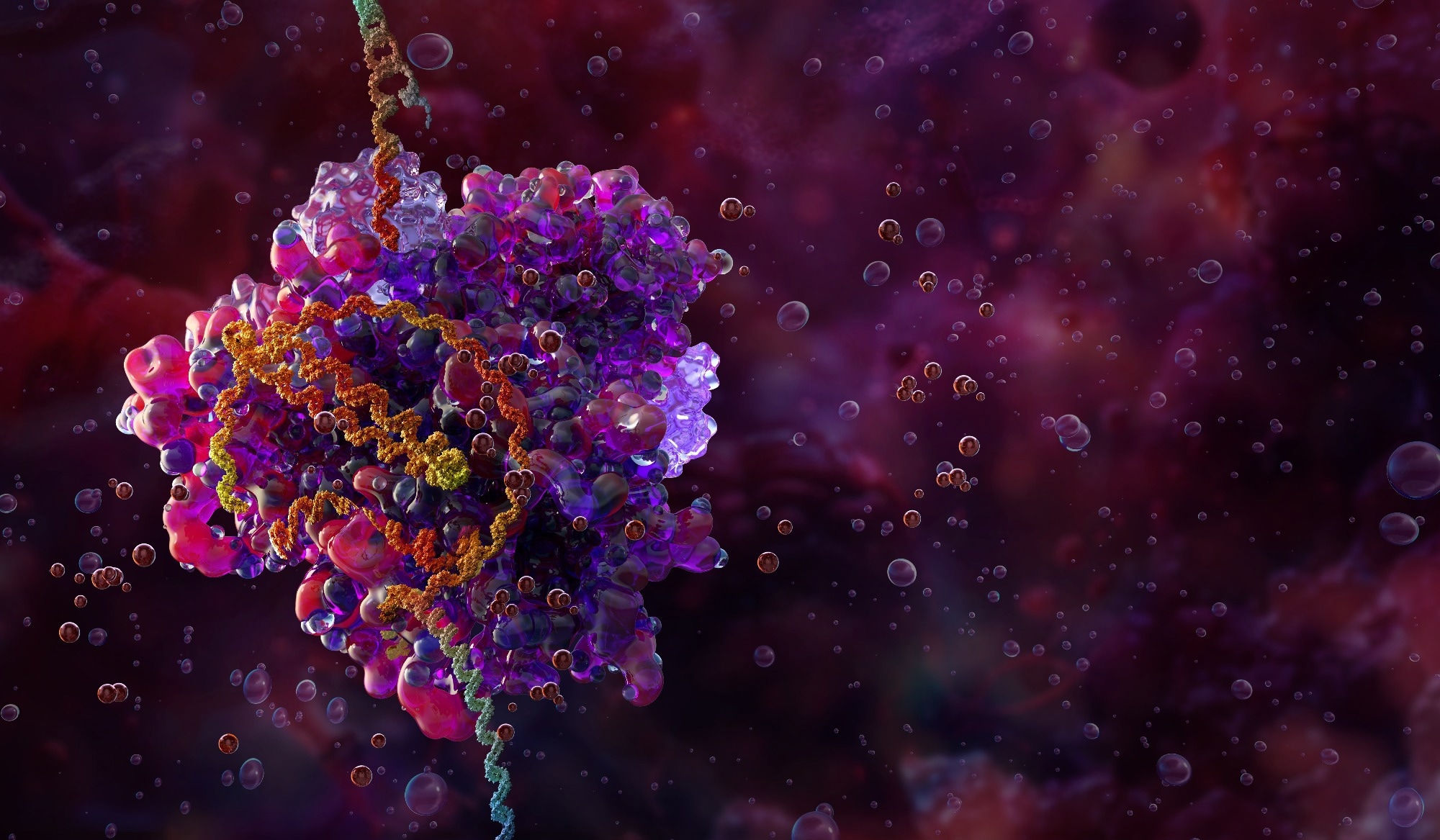
To address this, the researchers devised a unique delivery approach based on lipid nanoparticle technology, or LNPs. These minuscule “bubbles of fat,” pioneered by UBC researcher Dr. Pieter Cullis and brought to worldwide attention through mRNA vaccines, can carry gene-editing technologies to cells.
The researchers first make small, painless openings in the skin's outer layers using a clinically approved laser. This makes it possible for the lipid nanoparticles to cross the skin barrier and get to the skin stem cells that are located below the surface. After entering, the gene editor fixes the underlying DNA abnormality, allowing the skin to start acting more normally.
This is a highly targeted, localized approach. The treatment stays in the skin and we saw no evidence of off-target effects, which is a critical safety milestone.
Dr. Sarah Hedtrich, Study Senior Author and Associate Professor, School of Biomedical Engineering, University of British Columbia
The study was carried out in close cooperation with NanoVation Therapeutics, a Vancouver-based biotech company that is a UBC spin-off that focuses on creating genetic therapeutics based on LNP. The researchers have already begun collaborating with regulatory bodies to identify the required safety and effectiveness studies to get the medication into clinical testing.
“Our goal now is to take this from the lab into first-in-human clinical trials. We hope this work will ultimately lead to a safe, effective treatment that can transform the lives of patients who currently have no real therapeutic options,” concluded Dr. Hedtrich.
Source:
Journal reference:
Apaydin, D. C. et.al. (2026) Lipid nanoparticle-based non-viral in situ gene editing of congenital ichthyosis-causing mutations in human skin models. Cell Stem Cell. DOI: 10.1016/j.stem.2026.01.001. https://www.sciencedirect.com/science/article/abs/pii/S193459092600024X