 By Pooja Toshniwal PahariaReviewed by Lauren HardakerFeb 19 2026
By Pooja Toshniwal PahariaReviewed by Lauren HardakerFeb 19 2026By harnessing engineered helper T cells to target fibrillar amyloid, researchers demonstrate a dual strategy that clears dural deposits, remodels CNS immunity, and, using a transient mRNA approach, reduces parenchymal plaques in a preclinical Alzheimer’s model.
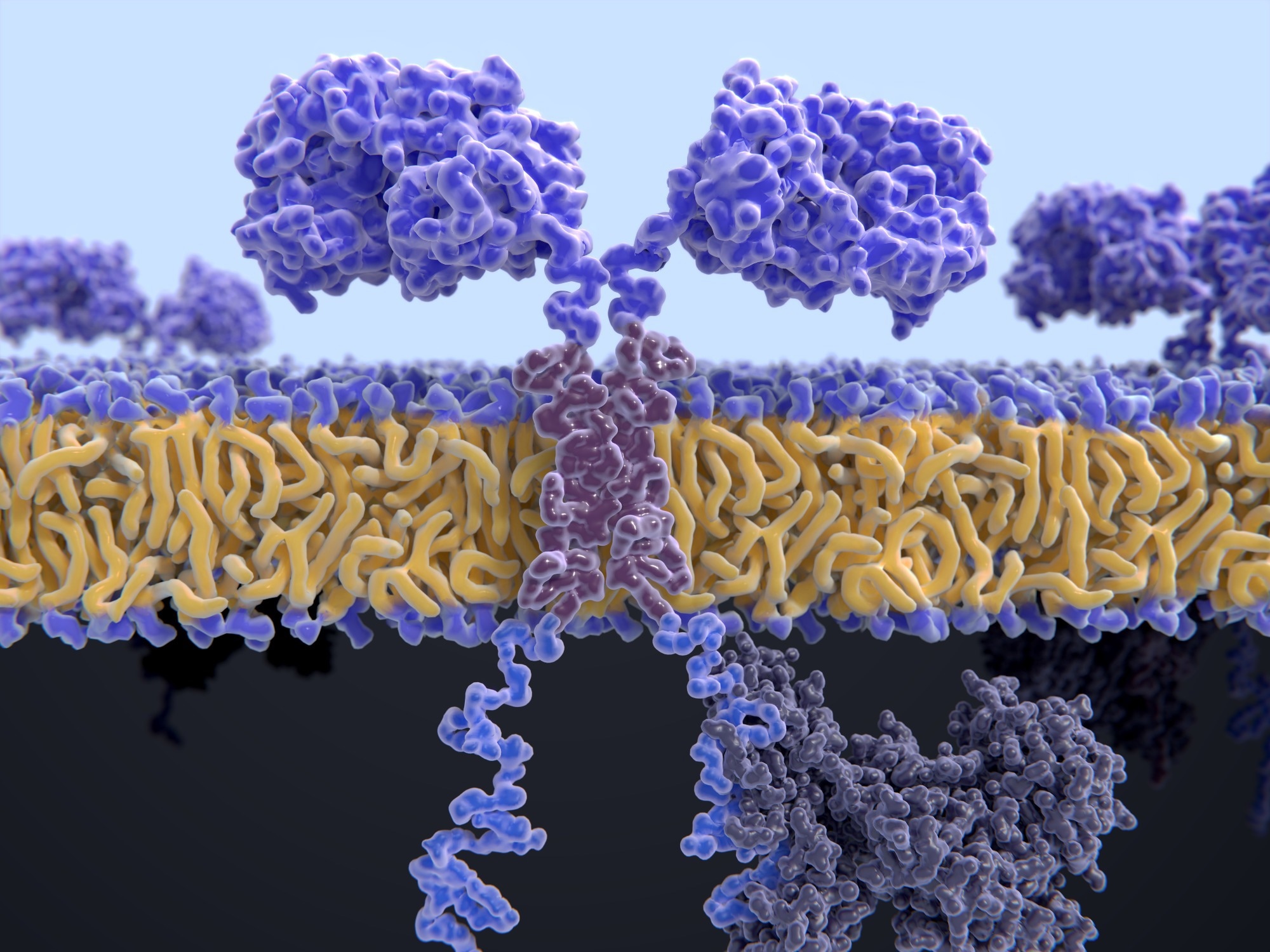 Image credit: Juan Gaertner/Shutterstock.com
Image credit: Juan Gaertner/Shutterstock.com
In a recent study published in Proceedings of the National Academy of Sciences, researchers describe a preclinical cellular immunotherapy approach for Alzheimer’s disease (AD). The team developed a cluster of differentiation 4 (CD4)+ helper T cells engineered to express chimeric antigen receptors (CARs) on their surface to specifically target amyloid-β (Aβ), associated pathology. These cells reduced Aβ deposits within the dura mater and were associated with immune changes that, depending on the CAR strategy used, extended to parenchymal brain pathology in mice.
In the stable retroviral CAR-T arm, plaque reduction was largely confined to the dura despite increased T cell infiltration into the brain parenchyma, whereas the transient mRNA CAR-T approach produced measurable reductions in parenchymal plaque burden. In addition, they promoted the recruitment of additional helper T cells in the central nervous system (CNS). The findings suggest that CAR T cell therapy could both modify disease pathology and remodel the immune environment in AD.
Limited Antibody Benefits Spur New Immunotherapy Approaches
AD remains the most prevalent form of age-related dementia worldwide. Aβ plaques, tau pathology, neuroinflammation, and progressive cognitive decline characterize AD. Antibody-based immunotherapies target amyloid; however, they offer modest clinical benefits and raise safety concerns, underscoring the need for alternative strategies.
Growing evidence suggests that T cells play a role in modulating disease development. Preclinical studies suggest that CD4+ subsets can reduce AD pathology by regulating neuroinflammation. However, human leukocyte antigen (HLA) diversity, T cell receptor specificity constraints, and safety issues observed in prior amyloid-directed immunization trials challenge clinical translation.
Lecanemab-Derived CAR Design Enhances Plaque Selectivity
In the present study, researchers used a murine model with 5 familial AD mutations (5xFAD) with established amyloid pathology to engineer CAR constructs targeting fibrillar Aβ aggregates to overcome the limitations of HLA-restricted T cell responses.
Using antibody sequences derived from Lecanemab and Aducanumab, the team identified the heavy (H) and light (L) chain regions and fused them into single-chain variable fragments (scFvs). They linked these to CD8 or CD28 hinges and transmembrane domains, followed by 4-1BB or CD28 costimulatory domains and the CD3 signaling region. The linkage generated multiple CAR configurations, which were screened; the most plaque-selective construct was selected based on signaling strength and specificity, while minimizing reactivity to monomeric or oligomeric amyloid species.
The researchers evaluated CAR functionality in nuclear factor of activated T (NFAT)-green fluorescent protein (GFP) hybridoma cells after retroviral transduction. Flow cytometry assessed activation in response to synthetic Aβ1–42 monomers, oligomers, or fibrils. The most selective construct, Lec28z, demonstrated strong activation in response to fibrillar Aβ and to brain samples of 5xFAD animals, but not wild-type controls.
Subsequently, the team transduced primary murine helper T cells using Lec28z or a control CAR and confirmed activation following exposure to Aβ fibrils. For in vivo studies, they adoptively transferred these CAR T cells into 5xFAD mice. Six weeks after transfer, they analyzed dural and brain tissues for T cell infiltration, plaque burden, and microglial activation using flow cytometry and immunostaining.
In addition, the researchers used transient messenger ribonucleic acid (mRNA) nucleofection of helper T cells to mitigate risks of prolonged activation and autoimmunity. They administered three doses over four weeks to mice, followed by immunohistochemical assessments of plaque load, astrogliosis, and dystrophic neurites.
CAR T Cells Accumulate At Dural Bridging Veins
Compared with aducanumab-based or 4-1BB variants, Lec28z induced robust signaling confined to fibrillar Aβ, with minimal reactivity to monomeric or oligomeric forms. In vitro, stimulation with Aβ fibrils led to receptor internalization and upregulated the activation markers, CD25 and CD69. The findings confirmed effective, plaque-specific engagement of CD4+ T cells.
Following adoptive transfer into 5xFAD mice, Lec28z CAR-expressing T cells preferentially localized to Aβ-rich regions of the dura mater, particularly at bridging veins within specialized immune entry points sometimes referred to as arachnoid cuff exit (ACE) sites. Following CAR T cell accumulation, the team observed recruitment of endogenous helper T cells and a marked decrease in dural amyloidosis, as demonstrated by whole-mount imaging and quantitative analyses.
Increased CD3+ T cell coverage correlated with reduced Aβ burden at individual bridging veins. While the stable retroviral CAR T cell regimen did not significantly alter parenchymal plaques, it led to significant helper T cell infiltration into the leptomeninges and brain parenchyma without increasing cytotoxic (CD8+) T cell numbers. Many CAR-expressing T cells acquired a central memory phenotype in draining lymph nodes, indicating activation and recirculation. However, enhanced microglial activation raised concerns about sustained immune stimulation.
Although CAR T cell accumulation correlated with reduced amyloid burden at these CNS border sites, the authors note that the precise mechanism of plaque reduction, whether through direct engagement of fibrillar deposits or through secondary cytokine-driven modulation of resident glia, remains unresolved.
The short-lived mRNA-modified CAR T cells addressed safety concerns. Mice treated with three doses over four weeks exhibited significant reductions in total parenchymal plaque load and dense-core plaques. In addition, the approach decreased astrogliosis, microgliosis, and dystrophic neurites. The findings suggest that transient helper T cells with CARs could mitigate multiple hallmarks of AD pathology while potentially limiting long-term immune-related risks. In contrast to the stable CAR approach, the transient mRNA strategy was associated with both reduced neuroinflammatory markers and measurable reductions in parenchymal amyloid burden.
Proof Of Concept For CD4 CAR Therapy In Alzheimer’s
The study findings provide proof of concept that amyloid-specific CAR-type helper T cells can be engineered to modify key features of Alzheimer’s disease. By selectively targeting fibrillar Aβ, these cells reduced AD pathology and reshaped the CNS immune environment by increasing CD4+ T cell recruitment and modulating glial activation states. The study also highlights the dura mater and its associated vascular, meningeal interfaces as an immunologically active gateway to the CNS in this model.
Importantly, transient mRNA-mediated CAR expression reduced neuroinflammatory markers and decreased parenchymal plaque burden in this preclinical model. This finding highlights a potentially safer and more adaptable therapeutic strategy. However, these findings remain limited to preclinical models, and further studies are required to determine safety, durability, and efficacy in humans.
Download your PDF copy by clicking here.
Journal Reference
Boskovic, P., Shalita, R., Gao, W., Vernon, H., Deng, Y. L., Colonna, M., Majzner, R. G., Amit, I., & Kipnis, J. (2026). Engineering chimeric antigen receptor CD4 T cells for Alzheimer’s disease. Proceedings of the National Academy of Sciences, 123(7), e2530977123. DOI: 10.1073/pnas.2530977123. https://www.pnas.org/doi/10.1073/pnas.2530977123