At the RIKEN Center for Integrative Medical Sciences in Japan, researchers under the direction of Hiroshi Ohno have found a connection between gut microbiota and the effectiveness of oral immunotherapy for milk allergies.
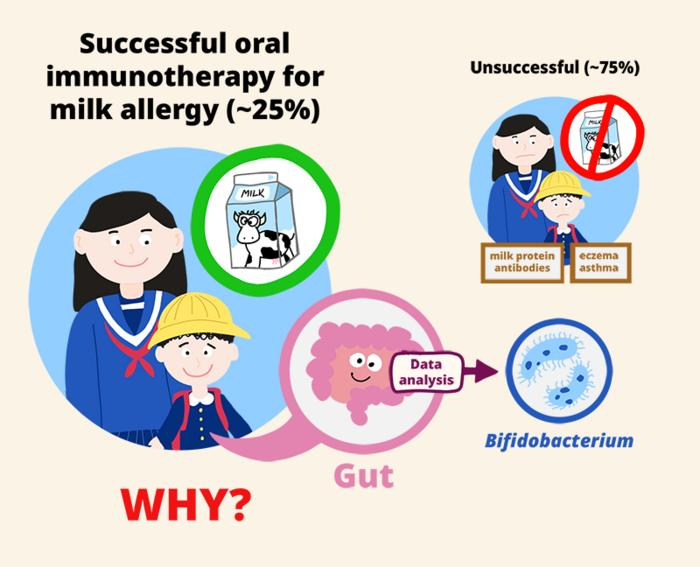 The study found that successful oral immunotherapy in children against milk allergy was associated with having Bifidobacterium bacteria in the gut, while unsuccessful treatment was associated with having eczema or asthma, and with high initial levels of milk-protein antibodies.
The study found that successful oral immunotherapy in children against milk allergy was associated with having Bifidobacterium bacteria in the gut, while unsuccessful treatment was associated with having eczema or asthma, and with high initial levels of milk-protein antibodies.
The study, which was published in the journal Allergology International, discovered a link between a higher likelihood of successful treatment and the genus Bifidobacterium, which is a beneficial bacterium found in the gut. The discovery could potentially aid in the creation of more potent oral immunotherapies, possibly in conjunction with probiotic supplements.
A lot of kids react allergic to cow’s milk, especially to certain proteins in the milk. While most recover, some people, especially those whose allergic reactions are severe enough to cause anaphylactic shock, find it very difficult to avoid foods containing milk for the rest of their lives. Researchers have discovered that oral immunotherapy, a procedure in which patients consciously consume small amounts of milk, improves milk allergy.
However, tolerance typically vanishes shortly after treatment ends, even though allergic reactions are managed during treatment.
Although the relationship between gut bacteria and oral immunotherapy for milk allergy is poorly understood, it is thought that these bacteria may help lessen allergic reactions to certain foods. Consequently, the RIKEN IMS team evaluated 32 kids who were allergic to cow's milk and were receiving oral immunotherapy; the initial month of the study was spent in a hospital.
Oral immunotherapy is not without risk. We closely monitored the children in the hospital, and in fact 4 children had such severe reactions to the milk that we could not allow them to continue the treatment.”
Hiroshi Ohno, Integrative Medical Sciences, RIKEN Center
After that, the remaining 28 kids finished a further 12 months of at-home therapy. They were then tested on a double-blind, placebo-controlled food challenge to see if they could still tolerate milk without experiencing any allergic reactions after going without it for two weeks. Children were initially given a very small amount of milk or placebo during the food challenge - just 0.01 ml - which was progressively increased every 20 minutes until they experienced an allergic reaction or were able to drink the remaining 30 ml without experiencing it.
The relationship between gut flora and successful treatment - defined as demonstrating milk tolerance that persisted beyond the treatment period by passing the food challenge - was the main focus of the researchers' analyses, along with immunological and bacterial changes that occurred during the treatment.
They discovered that during treatment, gut flora altered, and immunological markers for cow's milk allergy improved. Even though the 28 kids had been able to safely consume milk by the end of the treatment, only seven of them succeeded in passing the food challenge following the two weeks of milk restriction.
The team searched for the clinical characteristics and gut bacterial species associated with effective treatment to comprehend why the treatment was effective for these seven kids but not for the others. Among the clinical factors, children receiving treatment for eczema or asthma as well as those with initial higher levels of milk-protein antibodies were more likely to experience unsuccessful treatment.
A higher likelihood of a successful outcome from treatment was associated with the presence of Bifidobacterium, a genus of beneficial bacteria in the Bifidobacteriaceae family, among the gut bacteria.
During treatment, these bacteria only showed an increasing trend in the children who passed the final food challenge. This is good news when thinking about how to enhance oral immunotherapy because, unlike the first two factors, which are hard to modify, the types of bacteria in a person's gut are not fixed.
With this study, we have identified gut environmental factors that help establish immune tolerance against cow’s milk allergy via oral immunotherapy. The next step is to examine the mechanisms underlying this phenomenon and to develop ways to improve the effectiveness of oral immunotherapy, such as the addition of probiotic supplements.”
Hiroshi Ohno, Integrative Medical Sciences, RIKEN Center
Source:
Journal references:
Shibata, R., et al. (2024) Gut microbiota and fecal metabolites in sustained unresponsiveness by oral immunotherapy in school-age children with cow’s milk allergy. Allergology International. doi.org/10.1016/j.alit.2023.10.001