 By Pooja Toshniwal PahariaReviewed by Lauren HardakerJan 8 2026
By Pooja Toshniwal PahariaReviewed by Lauren HardakerJan 8 2026By preserving the natural architecture of fat tissue, researchers bypassed traditional stem cell methods to grow insulin-producing, bone marrow, and neural organoids, offering a scalable, preclinical blueprint for future regenerative therapies.
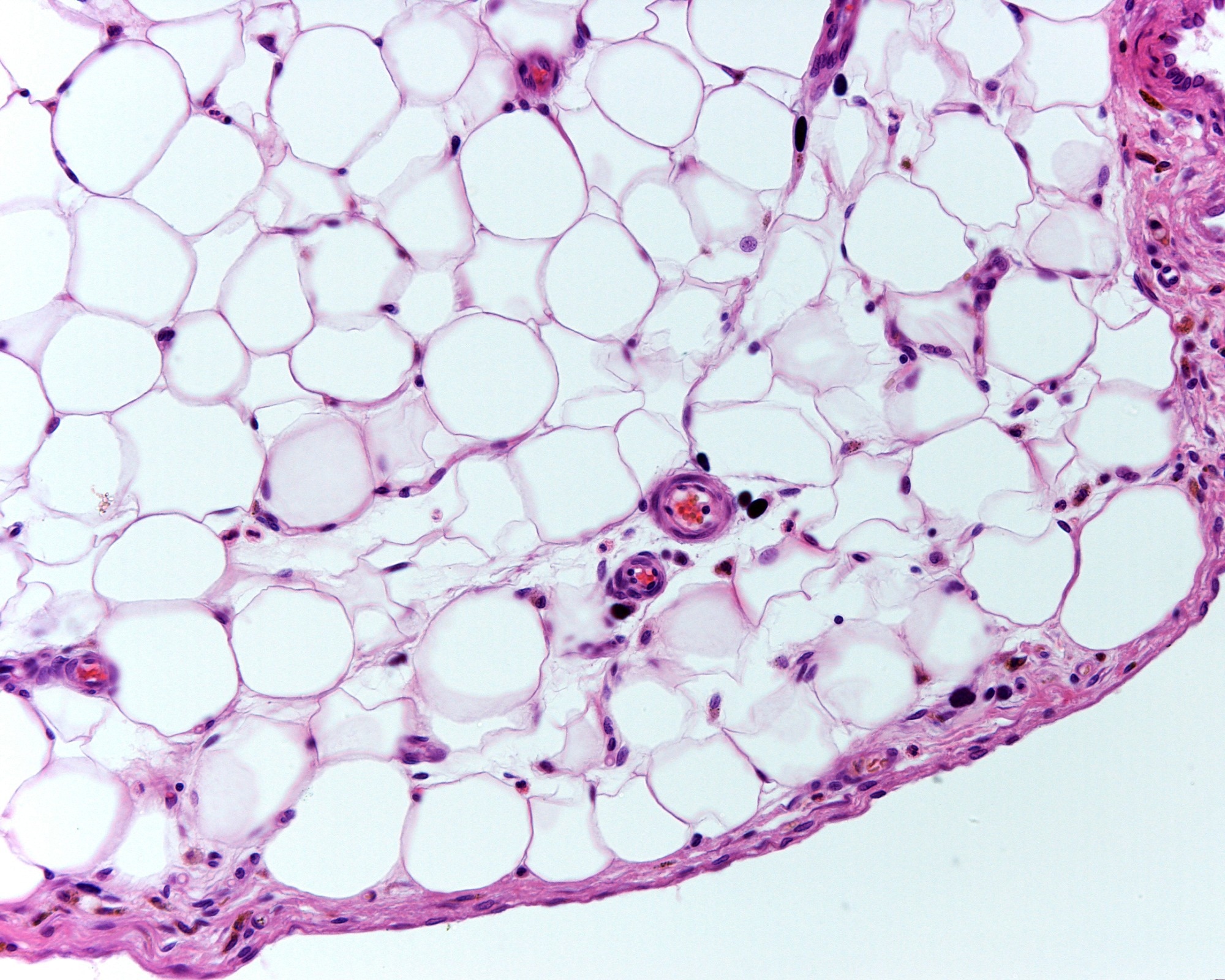 Image credit: Jose Luis Calvo/Shutterstock.com
Image credit: Jose Luis Calvo/Shutterstock.com
In a recent study published in Engineering, researchers investigated whether adult human adipose (fat) tissue can be directly converted into functional organoids representing multiple tissue types, with potential applications in regenerative medicine and diabetes treatment.
They found that preserving the tissue-level architecture in cultured fat tissue enabled the generation of bone marrow, insulin-producing, and neural-like organoids without the need for cell dissociation or genetic manipulation. In mouse models, these organoids restored insulin function, supported human blood formation following transplantation of human blood stem cells, and exhibited stable molecular and cellular organization.
Why Preserving Fat Tissue Architecture May Unlock Regeneration
The human body contains resident adult stem and progenitor cells embedded within specialized tissue niches. These microenvironments regulate cell fate, regeneration, and functional stability through complex interactions among extracellular matrix components, supporting cells, and biochemical cues.
Disruptions to native tissue architecture during conventional cell isolation and expansion procedures can impair stem cell function and limit clinical translation. Most current organoid-generation approaches rely on dissociated stem cells, extensive in vitro manipulation, and staged exposure to signaling factors, which raises challenges related to scalability, safety, and reproducibility.
Human adipose tissue is abundant, accessible, and known to contain multiple regenerative cell populations, making it an attractive candidate for developing alternative tissue-engineering strategies that better preserve native cellular context compared with conventional two-dimensional stem cell expansion systems.
A Tissue-Level Strategy Avoids Cell Dissociation and Gene Editing
Researchers aimed to develop a scalable, tissue-level method to generate functional organoids directly from adult human fat tissue. They used adipose samples obtained from liposuction procedures and mechanically processed them into microfat, which was then cultured in suspension to form reaggregated microfat (RMF) tissues.
Rather than isolating individual stem cells, the RMF tissues were allowed to self-organize over several weeks, preserving cell-cell interactions and extracellular matrix components. These RMF tissues were subsequently guided toward mesodermal, endodermal, and ectodermal lineages using defined culture conditions that mimic key stages of tissue development.
The study employed extensive in vitro characterization and in vivo transplantation experiments in immunodeficient mice. Techniques included histology, flow cytometry, and single-cell RNA sequencing as the primary molecular profiling approaches, as well as glucose-stimulated insulin secretion assays and long-term functional assessments following transplantation.
Functional Organoids Closely Resemble Native Human Tissues in Mice
RMF tissues differentiated into bone marrow-like organoids that, when implanted into mice, formed vascularized structures capable of supporting normal human hematopoiesis after engraftment of transplanted human CD34-positive blood stem cells.
RMF-derived insulin-producing islet organoids contained transcriptionally mature β-like cells, secreted insulin in response to glucose, and reversed hyperglycemia in streptozotocin-induced diabetic mice. Removal of the grafts caused blood glucose levels to rise again, confirming that glycemic control was graft-dependent.
Although undifferentiated RMF tissue did not improve metabolic outcomes, differentiated islet organoids maintained long-term glucose control for weeks to months without evidence of tumor formation.
At the molecular level, single-cell and complementary molecular analyses showed that RMF-derived organoids closely resembled native human tissues, including pancreatic endocrine cell populations and bone marrow niche components. Insulin-secreting cells exhibited gene expression patterns associated with maturation, metabolism, and hormone secretion.
In addition, RMF tissues were successfully converted into neural-like structures that express neuronal and glial markers in vitro, demonstrating their differentiation capacity across all three germ layers.
Intact Human Fat Offers a Scalable Path to Organoids
This study suggests that adult human adipose tissue can serve as a versatile and clinically relevant source for generating multiple types of functional organoids. By preserving tissue integrity and native microenvironments, this approach avoids many of the limitations of traditional stem cell-based organoid systems, which depend on prolonged cell expansion and reprogramming.
Compared with conventional cell-dissociation methods, tissue-level organoid generation supported stable differentiation, functional integration after transplantation, and durable physiological effects in preclinical models, including restoration of insulin-dependent glucose regulation.
A key strength of the study is its integrated tissue-engineering strategy combined with rigorous in vivo functional validation. However, the findings are currently limited to preclinical mouse models, and translation to human therapy will require further safety, durability, and scalability studies.
Overall, the findings highlight direct organoid generation from intact adult tissues as a promising avenue for regenerative medicine, with potential implications for diabetes treatment, hematopoietic support, and tissue replacement therapies if validated in future human studies.
Reference
Harmsen, J., Habets, I., Biancolin, A.D., Lesniewska, A., Phillips, N.E., Metz, L., Sanchez-Avila, J., Kotte, M., Timmermans, M., Hashim, D. de Kam, S.S., Schaart, G., Jörgensen, J.A., Gemmink, A., Moonen-Kornips, E., Doligheid, D., van de Weijer, T., Buitinga, M., Haans, F., De Lorenzo, R., Pallubinsky, H., Gordijn, M.C.M., Collet, T., Kramer, A., Schrauwen, P., Dibner, C., Hoeks, J. (2025). Natural daylight during office hours improves glucose control and whole-body substrate metabolism. Cell Metabolism 38(1). DOI: 10.1016/j.cmet.2025.11.006. https://www.cell.com/cell-metabolism/fulltext/S1550-4131(25)00490-5