 By Pooja Toshniwal PahariaReviewed by Lauren HardakerFeb 12 2026
By Pooja Toshniwal PahariaReviewed by Lauren HardakerFeb 12 2026A bone-building hormone may do more than strengthen skeletons. This study reveals how parathyroid hormone rewires degenerating vertebral endplates to reduce pathological nerve growth and ease chronic low back pain at its structural source.
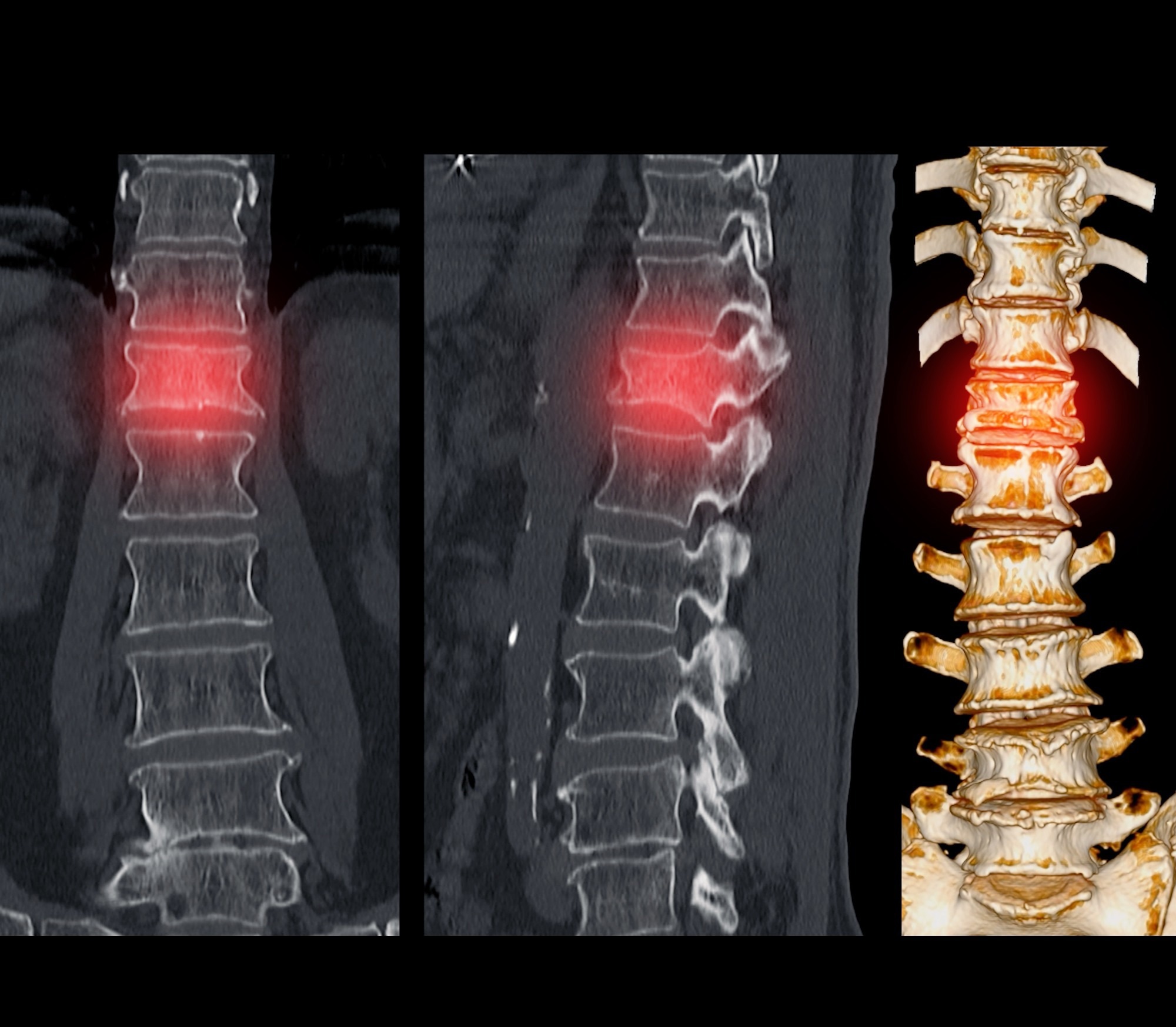 Image credit: Radiological imaging/Shutterstock.com
Image credit: Radiological imaging/Shutterstock.com
In a recent study published in Bone Research, researchers report that parathyroid hormone (PTH) therapy in preclinical models may represent a novel strategy for treating low back pain (LBP) associated with spinal degeneration.
Bone hormone curbs nerve overgrowth in spine
In mouse models, PTH improved degenerative vertebral endplate microarchitecture, including lower porosity and pore space, and reduced pain-related behaviors by limiting aberrant sensory nerve ingrowth within the vertebral endplate and vertebral body. These analgesic effects were linked to increased osteoblast-derived Slit guidance ligand 3 (Slit3), a neuronal guidance factor.
Together, the findings suggest that PTH may offer a potential therapeutic approach that targets both structural degeneration and axon guidance, mediated nociceptive innervation in degenerative spine disorders, although validation in human studies is required.
Chronic LBP increases with age as the spine undergoes progressive degenerative changes. Beyond intervertebral disc deterioration, aging drives structural and cellular alterations in vertebral endplates, including calcification, increased porosity, sclerosis, and dysregulated sensory innervation. These changes amplify nociceptive signaling and contribute directly to pain.
Current treatments largely focus on symptom relief rather than underlying pathology. Understanding how spinal degeneration promotes maladaptive nociceptive innervation provides a critical framework for evaluating mechanism-based therapies, such as parathyroid hormone treatment, aimed at restoring tissue integrity and alleviating pain at its source.
Three mouse models test PTH therapy
In the present study, researchers investigated whether PTH could alleviate low back pain by reducing pathological sensory nerve invasion and improving bone remodeling in degenerating vertebral endplates.
The study included three murine models of spinal degeneration: naturally aged mice, young mice subjected to surgery for lumbar spine instability (LSI) to model mechanical degeneration, and SM/J mice representing genetically accelerated aging. The animals received daily intraperitoneal injections of PTH (40 μg/kg) or vehicle for two weeks to two months, depending on the model.
The team assessed treatment outcomes at six months, eight months, and 24 months for the LSI, SM/J, and aged mice, respectively. They performed micro-computed tomography (micro-CT) to evaluate vertebral endplate structure at the fifth lumbar vertebra (L5). They conducted behavioral tests to assess pain-related outcomes. The tests included the Hargreaves assay for thermal sensitivity, the von Frey test for mechanical nociception, and voluntary wheel running to measure functional activity.
The researchers examined sensory innervation by quantifying protein gene product 9.5 (PGP9.5) and calcitonin gene-related peptide (CGRP) positive nerve fibers in vertebral bodies and endplates, and CGRP in dorsal root ganglia (DRG). Mechanistic analyses focused primarily on the aged and LSI models, as SM/J mice were excluded from certain mechanistic assays due to their complex genetic background. They performed osteoblast-specific deletion of the PTH receptor (PPR) to identify the cell type mediating nerve modulation and quantitative polymerase chain reaction (qPCR) to assess genetic expression of neuronal guidance factors.
Further, the team performed in vitro studies using pre-osteoblastic MC3T3 cells and primary osteoblasts to assess PTH-induced Slit3 expression. They also performed DRG neuron co-culture and microfluidic assays to evaluate nerve repulsion. Chromatin immunoprecipitation confirmed transcriptional regulation, and experiments involving osteoblast-specific Slit3 knockout mice validated its functional role in vivo.
PTH improves BV/TV and reduces porosity
PTH treatment consistently improved structural and pain-related outcomes across all three spine degeneration models. Micro-CT analysis showed that PTH increased BV/TV (bone volume fraction) while decreasing total porosity and pore space at the L5 endplate, with morphological improvements evident within one month in aged and LSI mice, and after two months in the SM/J group.
Behavioral assessments mirrored these structural findings. In the aged animals, PTH improved pressure tolerance, increased spontaneous wheel-running activity, and prolonged thermal withdrawal latency. After two months, the team observed similar improvements in mechanical and thermal pain sensitivity and functional activity in the LSI and SM/J groups.
These improvements were accompanied by a marked reduction in pathological sensory innervation. PTH decreased the length and protein expression of nerve fibers expressing CGRP and PGP9.5 in DRG and vertebral endplates, along with reduced expression of other sensory markers, including tyrosine hydroxylase and isolectin B4 (IB4).
Mechanistically, PTH selectively increased osteoblast-derived Slit3 expression. While several neuronal guidance factors were elevated, Slit3 was the only factor consistently upregulated across aging and degeneration models. In vitro, PTH induced dose-dependent Slit3 expression in osteoblasts, and conditioned media from PTH-treated osteoblasts suppressed DRG axon growth, an effect partly blocked by Slit3 neutralization and confirmed in vivo.
Genetic deletion of the PTH receptor or Slit3 in osteocalcin-expressing cells abolished the structural and behavioral benefits of PTH. Transcriptional analyses further showed that PTH enhanced Slit3 expression predominantly through forkhead box protein A2 (FoxA2) activation, identifying a direct osteoblast, nerve signaling pathway underlying pain relief in spinal degeneration.
Journal Reference
Zhang, W. et al. (2026). PTH induced osteoblast Slit3 to decrease aberrant sensory innervation in degenerated vertebral endplates to relieve low back pain in mice. Bone Research, 14(1), 12. DOI: 10.1038/s41413-025-00488-z. https://www.nature.com/articles/s41413-025-00488-z